Fluoroscopy-Assisted C1–C2 Posterior Fixation
for Atlantoaxial Instability
If neck pain becomes more severe, interferes with daily activities, or is accompanied by swelling and redness, it’s crucial to consult a healthcare professional. At Complete Orthopedics, our expert team specializes in addressing neck problems with customized treatment plans and surgical solutions. We focus on understanding your symptoms, identifying the underlying causes, and recommending the most suitable treatments or surgeries.
Our clinics are conveniently located throughout New York City and Long Island, and we have affiliations with six top hospitals, ensuring you receive the highest quality care for neck conditions. Schedule an appointment with one of our orthopedic surgeons online or by phone. Learn about the causes and treatments for neck pain and understand when surgery might be necessary.
Overview
Odontoid fractures, arthritis, and cervical tumors are among the possible factors that may lead to Atlantoaxial Instability. Failure to treat the destabilized atlantoaxial segment can result in abnormal translational and rotational movements that may cause neck pain and increase the likelihood of spinal cord compression.
Surgical Techniques for Stabilization
Both the atlantoaxial transarticular screw (TAS) technique and the screw and rod construct (SRC) technique can achieve atlantoaxial stability without requiring external immobilization. If the screws are placed too far to the side during the procedures, the atlantoaxial transarticular screw (TAS) technique and the screw and rod construct (SRC) technique could lead to vertebral artery injury (VAI) or spinal cord injury, respectively.
Although navigated surgery has demonstrated significant benefits, its adoption for spine surgery has been slower compared to cranial applications. This is partly because the setup of spinal navigation devices is relatively complex and time-consuming.
Effectiveness of Non-Navigated Posterior C1-C2 Fixation
Treating cervical instability and pain through non-navigated posterior C1-C2 fixation, employing both TAS and SRC, has been proven to be an effective treatment. The median operating room (OR) time for SRC may be slightly longer than that of TAS, but this can vary. The surgical time can be influenced more by user experience and surgical technique rather than the implementation of navigation technology itself.
Blood Loss Considerations
The amount of blood loss is typically less for the atlantoaxial transarticular screw (TAS) technique compared to the screw and rod construct (SRC), which is to be expected as TAS is a minimally invasive approach. The variation can be further clarified by the harm caused to the venous plexuses during the dissection required for the placement of the C1 screw. Incorporating navigation technology can potentially lower blood loss for both surgical methods. One possible explanation for this is that a less invasive approach is utilized, which leads to reduced handling near the cervical venous plexuses.
Risks of Vertebral Artery Injury
Vertebral artery injury is a widely recognized and hazardous complication linked with screw malpositioning in both TAS and SRC procedures, although the probability of this happening is very low. Changes in the screw’s initial position can have an effect on the precision of C1 screw placement. Sacrificing the C2 nerve root leads to fewer screws being misplaced. By using a study aided by fluoroscopy, a high level of precision can be attained, which can be assessed by postoperative CT scans.
One of the key reasons to consider using surgical navigation in cervical spine surgery is to prevent potential complications like vertebral artery injury (VAI) during instrumentation. While surgical navigation cannot entirely eradicate this risk, it has demonstrated advancements in screw precision as compared to non-navigated free-hand procedures.
Other techniques that can be employed to prevent vertebral artery injury (VAI) include the utilization of probing technologies that are based on Doppler, impedance, or optical properties. In the intervention group, Doppler probing can be conducted during lateral dissection, as well as stepwise drilling and tapping, to prevent vertebral artery injury (VAI). This technique is a valuable resource for both fluoroscopy-assisted and navigated C1-C2 surgical procedures.
Innovative Technologies
The Pediguard, an electronic conductivity device (manufactured by SpineGuard, Paris, France) that aids in the placement of pedicle screws, has been utilized in fluoroscopy-assisted cadaveric procedures to prevent vertebral artery injury (VAI). An optical technique called Diffuse Reflectance Spectroscopy has been incorporated into a surgical device to identify potential cortical breach during the insertion of pedicle screws.
Future Directions
The advancement and integration of innovative supportive technologies offer a potential to enhance the safety of all types of spinal surgeries involving instrumentation. Until the implementation of supportive technologies, experienced surgeons may consider non-navigated C1-C2 fixation as a viable choice for stabilizing the atlantoaxial segment. Posterior stabilization of C1-C2 with both transarticular screw (TAS) and screw and rod construct (SRC) is a secure and efficient approach for treating atlantoaxial instability, which typically results in pain relief in most cases.
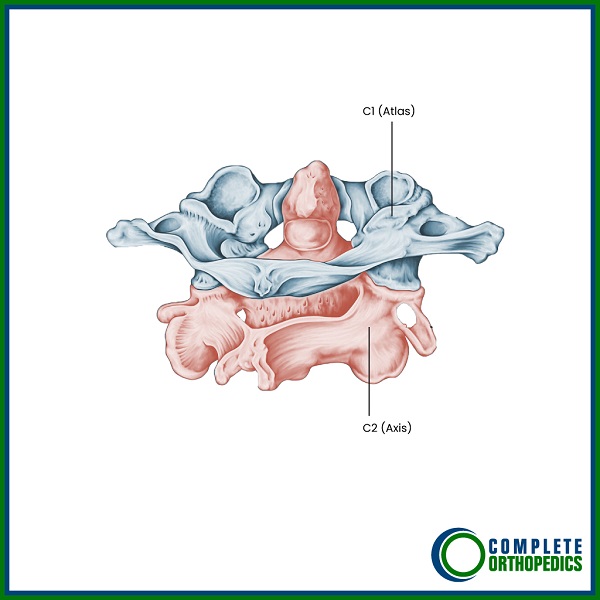
C1-C2 Facet Joint Illustrated
Affordability & Insurance
Planning surgery can feel overwhelming — but understanding your insurance doesn’t have to be. Here’s a simple breakdown to help you feel confident and prepared.
How Medicare Covers Fluoroscopy-Assisted C1–C2 Posterior Fixation
If you have Medicare, your healthcare provider may bill for CPT Code 22595 —this refers to a surgical procedure to stabilize the upper neck bones (C1 and C2) using screws and rods, guided by real-time X-ray imaging (fluoroscopy), to treat instability and prevent abnormal movement.
Medicare Coverage Overview
Medicare Part B typically covers 80% of the Medicare-approved amount for this procedure once you’ve met your deductible. That means most of the cost is taken care of — but you may be responsible for the remaining 20% – unless you have secondary insurance.
“What Will It Cost You?”
If you don’t have secondary insurance, here’s what you can expect:
Estimated Out-of-Pocket Cost for Posterior C1–C2 Fusion with Fluoroscopy (63020): $378.74
Could Additional Procedures Be Needed?
Sometimes, your surgeon may need to perform extra procedures to ensure the best outcome. If that happens, here’s what it could mean for your costs:
22853 (Placement of a supportive implant between spine bones to help them fuse properly) You pay $156.34
22840 (Use of rods or other devices to stabilize one level of the spine from the back) You pay $455
76000 (Real-time Xray) You Pay $24.84
For example, Lisa had neck pain and numbness in her arm due to a pinched nerve and spinal instability. Her surgeon first relieved the pressure on the nerve by removing part of the bone at one level (63020). To support her spine and help the bones fuse, they inserted a spacer between the vertebrae (22853) and stabilized it with rods from the back (22840). Fluoroscopy, or real-time X-ray (76000), was used during the surgery to guide proper placement. Medicare covered most of the procedure, and her secondary insurance helped cover the rest!
A Real-World Example
Imagine your surgery includes all three procedures:
To Stabilize the upper neck bones→ $387.74
Implant to fuse properly → $156.34
Use of rods or other devices to stabilize one level→ $455
Real-time xray while procedure → $24.84
Total Estimated Patient Cost: $1020.92
Have AARP or Another Secondary Insurance?
Good news!
If you carry a secondary insurance plan like AARP, it often covers your Medicare coinsurance — which means you may owe nothing out of pocket.
Plans vary, so it’s smart to check with your insurance provider to confirm exactly what they cover.
Injured at Work? Here’s How Workers’ Compensation Helps
If your spine surgery is related to a workplace injury, workers’ compensation insurance usually covers 100% of your medical costs — including your surgery, hospital stay, follow-ups, and rehabilitation.
- No deductibles
- No copays
- No out-of-pocket expenses
As long as your surgery is approved as work-related, your employer’s insurance handles everything so you can focus fully on your recovery.
Hurt in a Car Accident? No-Fault Insurance Protects You
If your cervical surgery is related to a motor vehicle accident, no-fault insurance usually covers all your medical expenses.
It doesn’t matter who was at fault — you’re covered for:
- Surgery costs
- Hospital charges
- Physical therapy
- Follow-up care
- No out-of-pocket costs in most cases.
- Peace of mind while you heal.
Need Help Navigating Insurance?
Insurance can seem complicated, but it doesn’t have to be overwhelming — we’re here to help you every step of the way.
Got questions? Call us today at (631) 981-2663
We’re happy to check your coverage, answer your questions, or even speak directly with your insurance company on your behalf.
Your focus should be on healing — let us handle the rest.
Do you have more questions?
What are the primary causes of Atlantoaxial Instability?
Odontoid fractures, arthritis, and cervical tumors are the primary causes of Atlantoaxial Instability.
What are the consequences of untreated Atlantoaxial Instability?
Untreated Atlantoaxial Instability can lead to abnormal translational and rotational movements, resulting in neck pain and an increased risk of spinal cord compression.
What surgical techniques are used to achieve atlantoaxial stability?
The atlantoaxial transarticular screw (TAS) technique and the screw and rod construct (SRC) technique are used to achieve atlantoaxial stability.
What are the risks associated with TAS and SRC procedures?
Why has the adoption of navigated surgery been slower for spine surgery compared to cranial surgery?
The setup of spinal navigation devices is relatively complex and time-consuming, contributing to slower adoption.
Is non-navigated posterior C1-C2 fixation effective in treating cervical instability and pain?
Yes, non-navigated posterior C1-C2 fixation, employing both TAS and SRC, has been proven effective.
How does the median operating room time compare between TAS and SRC techniques?
The median operating room time for SRC may be slightly longer than that of TAS, although this can vary based on user experience and surgical technique.
Which technique typically results in less blood loss, TAS or SRC?
The TAS technique typically results in less blood loss compared to the SRC technique.
What is a major complication associated with screw malpositioning in TAS and SRC procedures?
Vertebral artery injury (VAI) is a major complication, though its occurrence is very low.
What factors contribute to variations in blood loss during these surgeries?
Blood loss can be influenced by the harm caused to the venous plexuses during dissection for C1 screw placement and the use of navigation technology, which can reduce handling near the cervical venous plexuses.
How does the initial position of the screw affect the precision of C1 screw placement?
Changes in the initial screw position can affect the precision of C1 screw placement.
How can the precision of screw placement be assessed postoperatively?
Precision can be assessed using postoperative CT scans.
What is the benefit of sacrificing the C2 nerve root during these procedures?
Sacrificing the C2 nerve root can lead to fewer screw misplacements.
What is the role of surgical navigation in preventing complications during cervical spine surgery?
Surgical navigation helps prevent complications like vertebral artery injury (VAI) by improving screw precision.
Can surgical navigation entirely eliminate the risk of vertebral artery injury?
No, surgical navigation cannot entirely eliminate the risk but has shown advancements in screw precision compared to non-navigated procedures.
What other techniques can help prevent vertebral artery injury during surgery?
Techniques include the use of probing technologies based on doppler, impedance, or optical properties.
How is doppler probing utilized during C1-C2 surgical procedures?
Doppler probing is conducted during lateral dissection and stepwise drilling and tapping to prevent vertebral artery injury.
What is the Pediguard, and how is it used in spine surgery?
The Pediguard is an electronic conductivity device that aids in the placement of pedicle screws and has been used in fluoroscopy-assisted cadaveric procedures to prevent vertebral artery injury.
What is Diffuse Reflectance Spectroscopy, and how does it aid in surgery?
Diffuse Reflectance Spectroscopy is an optical technique incorporated into surgical devices to identify potential cortical breach during the insertion of pedicle screws.
What is the potential impact of integrating supportive technologies in spinal surgeries?
Supportive technologies can enhance the safety of spinal surgeries involving instrumentation.
What is the effectiveness of posterior stabilization of C1-C2 using TAS and SRC techniques?
Posterior stabilization using TAS and SRC techniques is secure and efficient, typically resulting in pain relief.
What should experienced surgeons consider until supportive technologies are widely implemented?
Experienced surgeons may consider non-navigated C1-C2 fixation as a viable choice for stabilizing the atlantoaxial segment.
What role does surgical experience play in the effectiveness of TAS and SRC techniques?
Surgical experience significantly influences the effectiveness and efficiency of TAS and SRC techniques.
What advancements have been made in screw precision for cervical spine surgery?
Advancements include the use of surgical navigation and probing technologies that improve the precision and safety of screw placement.
What are the benefits of minimally invasive approaches in these procedures?
Minimally invasive approaches, like TAS, often result in less blood loss and reduced handling near critical structures.

Dr. Nakul Karkare
I am fellowship trained in joint replacement surgery, metabolic bone disorders, sports medicine and trauma. I specialize in total hip and knee replacements, and I have personally written most of the content on this page.
You can see my full CV at my profile page.