Crepitus is a crunching or grating sound, or sensation felt in a joint on moving it. It is common in old age but not all joint crepitus signifies an underlying disease. However, when associated with pain or swelling joint crepitus usually denotes joint damage. Arthritis is a common cause of crepitus, especially among the elderly.
Joint Anatomy
A joint form where two bones meet, for example, a knee joint forms when the lower end of the thigh bone(femur) meets the upper end of the shinbone(tibia). Similarly, shoulder joint forms between the upper end of the arm bone and the socket formed by the shoulder blade. Besides the bones, numerous structures form a joint.
- Articular Cartilage: It is a smooth glistening white tissue covering the ends of bones forming a joint. It is tough yet flexible enough to cushion the gliding of the bones during movement. Additionally, it helps in reducing friction by acting as a slippery surface which allows for smooth movements of the joint.
- Ligaments: A tough tissue that connects two bones providing dynamic and static stability to a joint.
- Meniscus: A special form of cartilage present as a pad between the knee joint. In a normal weight-bearing joint such as the knee, forces as high as 8 times the bodyweight pass through it, meniscus acts as a shock absorber for the force.
- Muscles & Tendons: They provide structural as well as stabilizing support to the joints. In a knee, a joint large group of muscles, Quadriceps in the front and Hamstrings in the back provide constant support for the normal motion of the joint.
- Joint Capsule & Synovial Fluid: A Joint capsule seals the joint which contains synovial fluid. It is a thin clear sticky fluid that provides lubrication to the joints as well as provides nutrition to the cartilage.
Causes & Significance of Joint Crepitus
The sound which may be loud enough for others to hear or hushed could be due to a structure snapping over a joint which may be a tendon or ligament. More commonly it is due to grinding of the two joint surfaces as in arthritis. A popping sound due to the breaking of tiny bubbles in the joint is not a symptom of an underlying disease. However, crepitus which is associated with progressive pain or swelling should warrant a visit to a doctor.
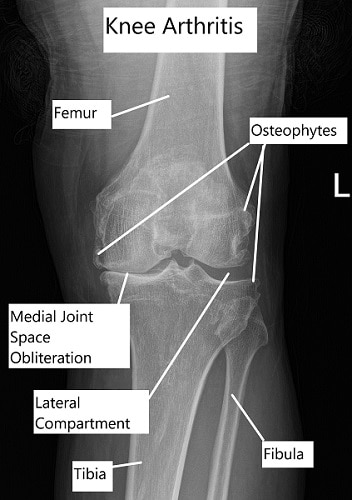
X-ray showing advanced knee arthritis
Causes of Arthritis
Age-related wear and tear arthritis called osteoarthritis or degenerative arthritis is a common source of joint crepitus in advancing age. Some other causes of arthritis are Rheumatoid Arthritis, Psoriatic Arthritis, and Gout.
Crepitus in Osteoarthritis (OA)
With degenerative changes in the joint, the articular cartilage erodes causing the bones to grind against each other. The constant grinding causes pain and crepitus. OA involves all the tissues forming a synovial joint including articular cartilage, muscles, bones, joints capsule and ligaments.
- Primary OA: It occurs without any specific underlying cause but increasing age and obesity are risk factors. Also, it tends to occur more often in women.
- Secondary OA: Any disease or injury which damages the structures forming the joint especially the articular cartilage will lead to osteoarthritis. Causes could be Rheumatoid arthritis, malalignment of joints, tendon or ligament injuries, gout, diabetes mellitus, intraarticular bleeding in hemophilia, acromegaly, Injuries to the cartilage, etc.
Stages of OA
- Early Stage: Initially the cartilage which undergoes increasing wear and tear with age is swollen. Cartilage is formed by vital cellular structures maintaining a balanced ratio of chemicals for its proper functioning. The balance is lost with age and the initial swelling progresses to fissures or cracks in the cartilage. The body unsuccessfully tries to form new cartilage with an increased blood supply.
- Intermediate Stage: The new blood vessels invade the bone underlying the articular cartilage called subchondral bone and increase its size. The cartilage degradation continues till it breaks and either dissolves in the joint or come to lie as “loose bodies”. The bone thickening is especially more prominent towards the sides of the joint forming bone spurs.
- Late Stage: Articular cartilage is lost with a thickened and swollen underlying bone. Cysts or cavities develop in the bone and the synovial tissue increases in size due to swelling. An increased amount of pressure exists in the joints.
Symptoms
Primary arthritis can involve several joints such as hands, shoulders, hips or knees but symptoms are not always consistent but they may come and go. There may be flare-ups or periods of remission. But the symptoms are always progressive i.e they get worse and their frequency increase with time.
- Pain: A sharp or dull persistent pain exists which is localized to one side or the entire joint. The pain gets worse at the end of the day due to activity. In the case of the knee, it may be particularly more with movements that strain the joint such as squatting or running up the stairs. At times the pain may flare up, severely restricting the joint movements.
- Crepitus: The squeaking sound occurs due to the rubbing or grinding of the bare subchondral bones in the joint. A broken cartilage peace may also rub between the joint surface and produce crepitus. In knees, the meniscus pads get torn in the process of OA and ongoing degeneration may produce the sound as well as locking. With the protective articular cartilage lost the joint no longer glides smoothly but instead grinds akin sandpaper producing crepitus.
- Swelling: Acute swelling with redness and pain may signify infection or inflammation. The swelling is mostly OA is generalized and may be associated with stiffness.
- Stiffness: Typically stiffness of the joint is present in the morning or after prolonged periods of inactivity. The movements are restricted and the joint seems to move after some activity is initiated.
- Effect of weather: Certain flare-ups are more in cold weather. The increased pain and swelling is not due to the temperature but the air pressure outside, which decreases and leads to increased swelling inside the joint.
- Restriction of Activities: Joint movements are gradually lost and certain movements such as squatting or climbing stairs require great effort associated with pain. The muscles around the joint also become weak and frail secondary to decreased motion.
Diagnosis
- History: A detailed history regarding the onset of symptoms and associations is taken.
- Physical examination: Physicians perform various tests to check for the movements involved and the stability of a joint.
- Blood Tests: These are done to rule out systemic diseases such as rheumatoid arthritis, gout or infection.
- Imaging: X-ray is usually the first investigation done to check for joint space and thickening of the bones. For a detailed evaluation, a CT scan can be done but usually, an MRI is the most helpful investigation. It details all the structures inside the joint.
- Arthrocentesis: Joint aspiration or arthrocentesis involves taking a tiny amount of synovial fluid from the joint using a syringe. The contents of synovial fluid are then subjected to lab tests.
Management
It depends on the age, severity of disease and demands of the patient.
Non-Surgical
- Weight loss: It directly impacts the amount of load transmitted to the weight-bearing joints like the knee and hip. Bodyweight directly impacts the severity of symptoms.
- Lifestyle Moderation & Physical Therapy: Avoiding activities that strain the jointly provide relief. Strengthening of the muscles surrounding the joint provide stability and decrease the symptoms.
- Ice compression or Heat Pads: They provide significant relief especially during a flare-up. Gentle compression with rest and icing decreases pain and swelling
- Nonsteroidal Anti-inflammatory medications: These orals medications provide symptomatic pain relief and also decrease the swelling associated with OA. Certain side effects like gastritis, ulcers, and blood-thinning curtail their long term use.
- Others: Medications such as glucosamine, chondroitin sulfate, diacerein, and hyaluronic acid have been used but controversies surround their actual benefit.
- Intra Articular Steroid Injections: These are administered in the joint and decrease the inflammation associated with OA. Significant pain relief is obtained but the effects wear off after a few months. Repeat injections may be needed.
Surgical
- Arthroscopic debridement: Early stages of OA can be managed using an arthroscopic procedure. Using keyhole techniques a tiny camera is inserted along with instruments. All the dead tissues and loose bodies are removed.
- Osteotomy: Bone cutting surgery is done to change the alignment of the forces acting on the joint. It decreases the pressure on the area of the cartilage involved in OA. Helpful only in the early stages of the disease.
- Joint Replacement: Arthroplasty surgeries have revolutionized the treatment of osteoarthritis. The joint ends are replaced or resurfaced with metal and plastic parts. The prosthetic parts recreate the joint movements.
Excellent stability is achieved as the parts reduplicate the function of ligaments and meniscus. The alignment of the joint line is created as it was before the disease process. This provides a pain-free joint with a nearly normal range of motion.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
