Transforaminal Lumbar Interbody Fusion Surgery
The transforaminal lumbar interbody decompression surgery (TLIF) is a surgical technique used to fuse two adjacent vertebrae. The surgery involves a bone cage’s placement and a bone graft and implants (pedicle screws and rods) to stabilize the segment. The surgery may be performed with a traditional open technique or minimally invasive technique.
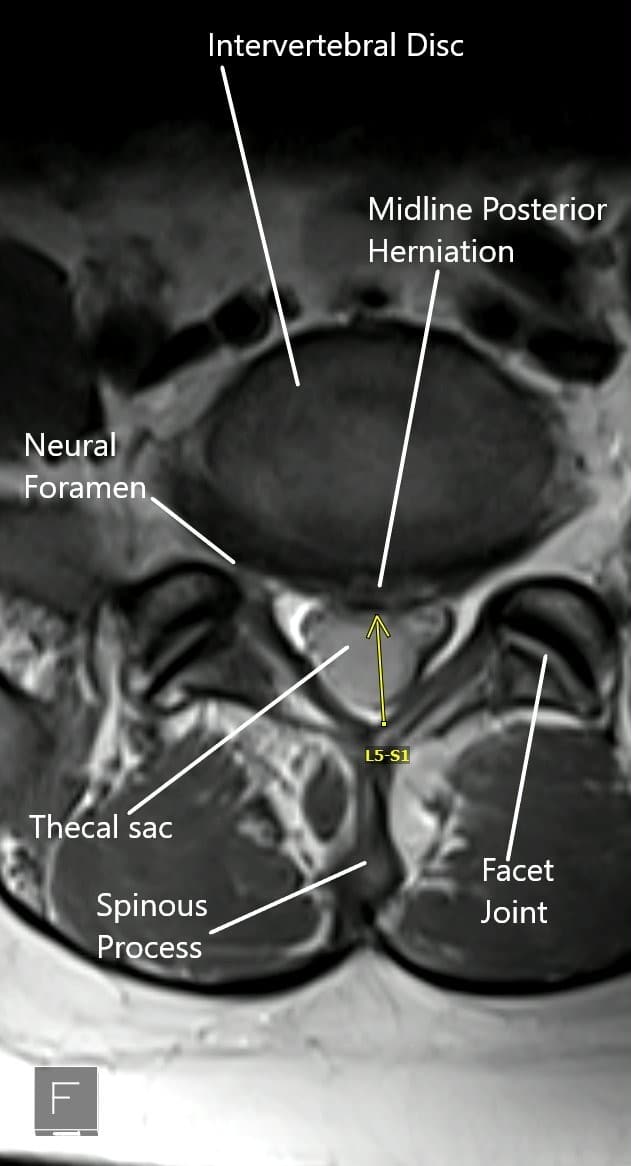
MRI of the lumbar spine in axial view showing central disc herniation.
Transforaminal Lumbar Interbody Fusion Surgery Indications
Lumbar fusion surgery is performed after all conservative management options have been tried without satisfactory results. Various conditions that may be treated with fusion surgery are:-
- Degenerative disk disease may cause symptoms of back pain and radiculopathy. With advancing age, there may be a loss of disk height resulting in subsequent segment instability. The body tries to re-align by enlargement of ligaments and bony structures that may impinge upon the neural structures.
- Recurrent intervertebral disc herniations may result after traumatic events or degenerative conditions. The herniated disk may compress the exiting or traversing nerve roots causing symptoms of radiculopathy.
- Spondylolisthesis occurs as a result of misplaced vertebrae due to developmental, isthmic, or degenerative causes. The displaced vertebrae may cause back pain and symptoms of radiculopathy or neurogenic compression.
- Spinal canal stenosis occurs as a result of narrowing of the vertebral canal or the neural foramen.
- Failed back surgery involves the continuation of symptoms of back pain or radiculopathy after prior spine surgery. The failure of surgery may be due to implant failure, adjacent level degeneration, wrong diagnosis, incomplete surgery, etc.
TLIF Procedure
The surgery is performed under general anesthesia, and the patient is placed on his/her abdomen. The surgeon gives a skin incision slightly towards the body’s side (about 4cm from the midline) over the involved segment. A metallic wire is passed under fluoroscopic guidance towards the facet joint complex.
Serial dilators are passed over the wire to create a muscle splitting rather than cutting exposure. The tubular retractors are then used to visualize the involved segment.
The surgeon then decompresses the segment by removing the facet joint and by performing laminectomy. The intervertebral disk material is removed from the involved side. Any other tissue compressing upon the neural tissue is removed.
The surgeon then introduces a cage between the involved vertebrae after the endplate preparation. The cage may be made of metal alloy or high-grade plastic such as PEEK (poly ether-ether ketone). The bone cage functions to maintain the disc space between the two vertebrae.
The bone cage is filled with bone graft material. The bone graft may be taken from the patient’s pelvis during the surgery or maybe utilized from a bone bank. The bone graft ensures speedy union between the vertebrae.
Mirror incisions are made on the other side to introduce pedicle screws. Rods are tightened over the pedicle screws to support the arthrodesis in the front. The screw and rod construct also decompress the vertebrae by distraction.
Throughout the surgery, care is taken to protect the nerve roots and the dural sac from inadvertent damage. The incisions are closed in layers, and the patients may go home after a day’s stay at the hospital or may go home the same day if a minimally invasive technique is used.
Transforaminal Lumbar Interbody Fusion Surgery Complications
Although the risk of complications remains relatively low, there may be potential complications of infection, blood loss, nonunion of the fusion, implant failure, blood clots, etc. The operating surgeon will discuss all the potential risks and complications with the patient before the surgery.
Transforaminal Lumbar Interbody Fusion Surgery Postoperative Care
The majority of the patients are advised to walk the next day of the surgery and resume their daily activities. They are advised against the lifting of heavyweights and sudden bending or twisting movements. Physical therapy is initiated to strengthen the back muscles and improve flexibility. Pain medications may be used in the initial postoperative period.
Benefits of TLIF
The transforaminal approach utilized the entry from the side of the back. The entry prevents cutting of the back muscles to reach the involved segment. The muscles and other soft tissues are instead separated with the use of tubular dilators. This has been shown to improve the postoperative recovery period.
Patients treated with the TLIF approach experience less postoperative pain and require fewer doses of pain medications. They can also participate in physical therapy earlier than the patients treated with the traditional posterior approach.
A large amount of bone graft can be placed from the side of the spine that ensures a steadier fusion. The retraction of the dural sac and the nerve roots is minimum, so the chances of nerve injury and dural tear are far less with the transforaminal approach.
The lateral trajectory used in the transforaminal approach can also be used in patients with prior spine surgery. The approach may be used in patients with far lateral disc herniations and instability.
Contraindications
The transforaminal approach is contraindicated in patients with metabolic bone disorders such as osteoporosis. The TLIF surgery is also not indicated in patients with disc infection, multilevel disease, extensive scarring from prior surgery. The approach is also not indicated in patients with complete disc involvement as through TLIF, the surgeon can reach only one side of the disc.
Do you have more questions?
What is the main goal of TLIF surgery?
The primary goal of TLIF surgery is to stabilize the spine and promote the fusion of vertebrae by reducing painful motion in the affected spinal segment, which helps relieve chronic pain caused by conditions such as degenerative disc disease or spondylolisthesis.
Who is a good candidate for TLIF?
Ideal candidates are individuals with chronic lower back pain or leg pain due to conditions like degenerative disc disease, spinal stenosis, or spondylolisthesis that have not responded to conservative treatments such as physical therapy or medication.
How is TLIF different from other spinal fusion surgeries like PLIF or ALIF?
TLIF uses a more lateral approach to access the disc space, reducing the need for nerve retraction compared to posterior lumbar interbody fusion (PLIF). Unlike anterior lumbar interbody fusion (ALIF), which requires an additional incision in the abdomen, TLIF achieves fusion through a single posterior incision.
Is TLIF a minimally invasive surgery?
TLIF can be performed as a traditional open procedure or using minimally invasive techniques. Minimally invasive TLIF involves smaller incisions, less muscle dissection, and a quicker recovery period, but the technique chosen depends on the patient’s specific condition.
What materials are used for the bone graft in TLIF?
Bone graft materials may include autograft (your own bone, typically from the iliac crest), allograft (donor bone), or synthetic bone substitutes. The choice depends on the patient’s situation and surgeon’s preference.
How long does the TLIF surgery take?
The length of the procedure varies based on the number of levels fused and whether it’s performed minimally invasively, but on average, TLIF takes about 2-4 hours.
What are the risks or complications associated with TLIF?
While TLIF is generally safe, potential complications include infection, nerve injury, blood clots, nonunion (failure of the bones to fuse), hardware failure, and persistent pain. However, many of these risks are minimized with proper surgical technique and post-operative care.
How much pain will I have after TLIF surgery?
While pain is expected in the immediate post-operative period, it is usually managed with medication. Most patients experience a reduction in their chronic back or leg pain over time as the spine stabilizes.
How soon after TLIF surgery can I walk?
Most patients are encouraged to start walking as early as the day after surgery or within 48 hours, depending on their comfort level and surgical outcome.
What kind of anesthesia is used for TLIF?
General anesthesia is typically used for TLIF surgery, meaning the patient will be completely unconscious during the procedure.
How long is the hospital stay after TLIF?
Patients typically stay in the hospital for 3 to 7 days after surgery, depending on their health condition and recovery progress.
Will I need a brace after TLIF surgery?
In some cases, a lumbar brace may be recommended to support the spine during the early stages of recovery, especially if significant bone loss or osteoporosis is present.
When can I return to work after TLIF?
This depends on the type of work you do. Patients with desk jobs may return to work within 4-6 weeks, while those with physically demanding jobs may need 3-6 months before returning to full activity.
What are the signs that the bone fusion was successful?
Successful fusion is usually confirmed through follow-up X-rays or CT scans showing solid bone formation between the vertebrae. Clinically, a reduction in pain and improved mobility are good indicators.
What happens if the bones don’t fuse properly after TLIF?
This is known as nonunion or pseudoarthrosis. In these cases, further treatment may involve bone stimulators, revision surgery, or other interventions to promote fusion.
Can TLIF be performed on multiple spinal levels?
Yes, TLIF can be performed on multiple levels if necessary, though it increases the complexity and length of the surgery.
Will I need physical therapy after TLIF surgery?
Yes, physical therapy is often an essential part of the recovery process. It helps strengthen the muscles around the spine, restore flexibility, and improve overall function.
Is TLIF effective for treating leg pain (sciatica)?
Yes, TLIF can be very effective for treating leg pain caused by nerve root compression, such as sciatica, by relieving pressure on the nerves and stabilizing the affected segment.
How long will it take to fully recover from TLIF?
Full recovery can take 6-12 months as the fusion progresses. During this period, patients will gradually return to their normal activities, guided by physical therapy and follow-up assessments.
What is the long-term success rate of TLIF surgery?
Studies indicate that 85-95% of patients achieve solid fusion and significant pain relief after TLIF. Long-term outcomes depend on factors such as patient compliance with post-operative care and avoidance of smoking, which impairs bone healing.
Is it safe to undergo TLIF if I’ve had previous spine surgery?
Yes, TLIF is often preferred for patients with previous spine surgery, as its lateral approach allows the surgeon to avoid areas of scar tissue that could complicate other fusion techniques.
What can I do to improve my chances of a successful outcome?
To improve your chances of success, it is crucial to follow your surgeon’s instructions closely. Avoid smoking, maintain a healthy diet rich in calcium and vitamin D, and participate in physical therapy as recommended.
Will I be able to resume sports or physical activities after TLIF?
Most patients can return to low-impact activities, such as walking or swimming, within 6-8 weeks. Higher-impact sports, like running or weightlifting, may take longer—up to 6-12 months—but should only be resumed after your surgeon gives clearance.
Will the hardware (screws and rods) need to be removed later?
In most cases, the hardware used in TLIF is permanent and does not need to be removed. However, in rare instances where the hardware causes discomfort or complications, removal may be considered after fusion is confirmed.
Can TLIF correct spinal deformities like scoliosis?
TLIF can be used to treat certain spinal deformities, such as spondylolisthesis or mild scoliosis, by realigning and stabilizing the spine. However, severe scoliosis may require more complex procedures.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
