Knee stiffness following knee replacement surgery is a common concern that can impede recovery and daily activities. While knee replacement surgery is widely successful in alleviating pain, stiffness may occur, affecting the patient’s ability to fully extend or flex the knee. At Complete Orthopedics, we specialize in diagnosing and managing post-surgical knee stiffness with personalized treatment strategies, including non-surgical and surgical interventions when necessary.
How Common It Is and Who Gets It? (Epidemiology)
Stiffness after knee replacement is a known complication, though it is relatively rare. It can affect patients of all ages but is more common in those who have undergone previous knee surgeries or have certain medical conditions such as rheumatoid arthritis, diabetes, or obesity. Stiffness is also more likely in individuals who experience complications during or after surgery, such as infection or improper physical therapy participation.
Why It Happens – Causes (Etiology and Pathophysiology)
Knee stiffness after replacement surgery can be caused by various intrinsic and extrinsic factors:
- Preoperative Factors: A history of previous knee surgery, limited range of motion before surgery, and multiple comorbidities like diabetes may increase the likelihood of stiffness post-surgery.
- Intraoperative Factors: Improper alignment of the knee prosthesis, incorrect sizing, excessive or inadequate bone removal, or failure to remove bone spurs can lead to stiffness.
- Postoperative Factors: Delayed participation in physical therapy, infection, heterotopic ossification (abnormal bone growth in tissues), or excessive blood thinner use can contribute to joint stiffness. Scar tissue formation (fibrosis) is also a significant cause of restricted movement.
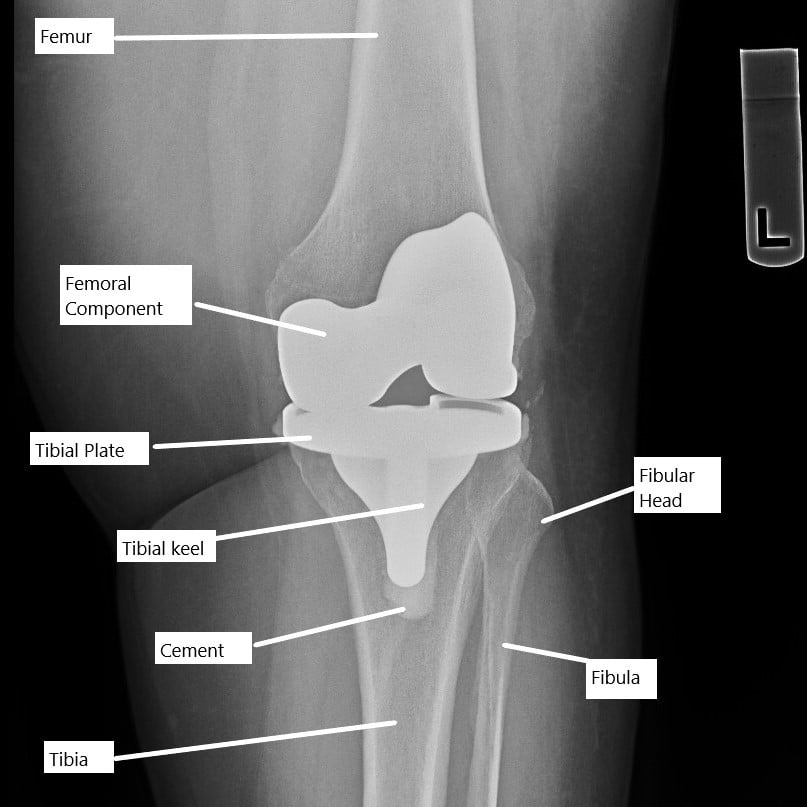
X-ray showing a total knee replacement.
How the Body Part Normally Works? (Relevant Anatomy)
The knee joint is a hinge joint that allows for the bending (flexion) and straightening (extension) of the leg. Knee replacement surgery involves replacing the damaged knee surfaces with a metal and plastic prosthesis to restore mobility. Normally, the knee can flex from 0 degrees (fully straight) to about 135 degrees (fully bent). After surgery, a proper range of motion (ROM) is essential for day-to-day activities, such as walking, sitting, or climbing stairs.
What You Might Feel – Symptoms (Clinical Presentation)
The primary symptom of post-surgery knee stiffness is the inability to fully bend or straighten the knee. This is quantitatively assessed by measuring the knee’s range of motion (ROM). Stiffness may be mild, with less than 90 degrees of flexion, or more severe if the knee cannot be straightened by more than 5-10 degrees. Pain, swelling, and difficulty in performing activities such as sitting or rising from a chair or climbing stairs are common complaints.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis of knee stiffness after surgery typically begins with a detailed physical examination, focusing on the knee’s range of motion. Imaging studies, including X-rays or CT scans, may be used to evaluate the alignment of the knee implant and detect any bone-related issues. If further complications are suspected, MRI may be used to assess soft tissues, including scar tissue or abnormal bone growth.
Classification
Knee stiffness after knee replacement can be graded based on the degree of movement:
- Mild Stiffness: Limited knee flexion (less than 90-100 degrees).
- Moderate Stiffness: Knee flexion between 70-89 degrees.
- Severe Stiffness: Knee flexion less than 70 degrees or inability to straighten the knee properly.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions that may present with similar symptoms include:
- Infection: Swelling, pain, and redness with limited movement may indicate an infection in the prosthetic joint.
- Implant Misalignment: If the prosthesis is not properly aligned, it may restrict knee movement.
- Adhesions or Scar Tissue: Abnormal tissue growth around the knee may restrict movement.
- Heterotopic Ossification: Abnormal bone formation in the soft tissues can cause stiffness and discomfort.
- Patellofemoral Pain Syndrome: If the kneecap is misaligned, it may cause pain and stiffness, particularly when bending the knee.

Intraoperative image of total knee replacement.
Treatment Options
Non-Surgical Care
For most cases of post-surgical knee stiffness, non-invasive treatments are the first line of management:
- Physical Therapy: Structured exercises focusing on strengthening the quadriceps and other muscles around the knee, as well as improving range of motion.
- NSAIDs: Nonsteroidal anti-inflammatory drugs like ibuprofen or naproxen can help manage pain and inflammation.
- Ice and Elevation: Applying ice to reduce swelling and elevating the leg can help improve comfort during the early stages of recovery.
- Continuous Passive Motion (CPM) Machines: These machines move the knee gently to maintain joint mobility and prevent stiffness.
Surgical Care
If non-surgical methods fail to improve stiffness, surgical interventions may be necessary:
- Manipulation Under Anesthesia (MUA): This procedure involves physically moving the knee under general anesthesia to break up scar tissue and improve flexibility. This is most effective within the first few months after surgery.
- Arthroscopic Lysis of Adhesions: In cases of excessive scar tissue, arthroscopic surgery can be used to remove fibrous adhesions and improve knee movement.
- Revision Knee Replacement: If stiffness is caused by implant misalignment or damage, a revision knee replacement may be performed to correct the issue.
Manipulation under Anaesthesia (MUA)
Manipulation under anesthesia is a non operative technique to manage knee stiffness following surgery. The manipulation is performed in patients who are unable to bend their knees less than 90 degrees. The manipulation has best results if performed in the first 3 months of the surgery.
During manipulation, the patient is put under general anesthesia. In general anesthesia, the patient sleeps while his/her muscles are relaxed. The surgeon then tries to physically bend or straighten the knee with an aim to break the fibrosis tissue adhesions.
Not all patients are candidates for manipulation under anesthesia as excessive manipulation may carry a risk of fracture or rupture of extensor mechanism (patella fracture, patellar tendon rupture, etc).
Recovery and What to Expect After Treatment
Recovery from knee stiffness varies depending on the severity of the condition and the type of treatment used:
- Conservative Management: With adequate physical therapy and rest, most patients experience gradual improvement within a few weeks to months.
- Surgical Recovery: After MUA or arthroscopic procedures, recovery typically involves a period of rest followed by physical therapy to restore knee function. Full recovery can take several months, and some patients may need ongoing rehabilitation.
Possible Risks or Side Effects (Complications)
Potential risks from knee stiffness treatment include infection, bleeding, and the risk of injury to the knee during manipulation. For surgical treatments, complications may include damage to surrounding tissues, nerve injury, or failure to achieve the desired range of motion.
Long-Term Outlook (Prognosis)
The long-term prognosis for knee stiffness after replacement is generally good, particularly when managed early. Most patients recover full or near-full range of motion, although a small percentage may experience persistent stiffness that requires further intervention. The prognosis is better when physical therapy is initiated early and adhered to consistently.
Out-of-Pocket Costs
Medicare
CPT Code 27570 – Manipulation Under Anesthesia (MUA – Knee): $37.21
CPT Code 29884 – Arthroscopic Lysis of Adhesions: $147.96
CPT Code 27487 – Revision Total Knee Replacement (Femoral + Tibial Components): $413.16
CPT Code 27486 – Revision Total Knee Replacement – Single Component: $332.04
Under Medicare, 80% of the approved amount for these procedures is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, leaving most patients with little to no out-of-pocket expenses for Medicare-approved knee surgeries. These supplemental plans work directly with Medicare to provide full coverage for the procedures.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, ranging from $100 to $300, depending on the specific policy and network status.
Workers’ Compensation
If your knee surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your knee injury resulting in surgery is caused by a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses, including manipulation under anesthesia, lysis of adhesions, and knee replacement revision surgeries. The only possible out-of-pocket cost may be a small deductible depending on your individual policy terms.
Example
David, a 60-year-old patient with knee stiffness after a prior knee replacement, underwent manipulation under anesthesia (CPT 27570) and later required revision total knee replacement (CPT 27487). His estimated Medicare out-of-pocket costs were $37.21 for the manipulation and $413.16 for the total knee replacement revision. Since David had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for the surgeries.
Frequently Asked Questions (FAQ)
Q. What causes stiffness after knee replacement?
A. Stiffness can result from factors such as scar tissue formation, implant misalignment, inadequate post-surgery physical therapy, or infection.
Q. Can physical therapy help with stiffness after knee replacement?
A. Yes, physical therapy plays a crucial role in improving range of motion and strength after knee replacement. It is essential to start therapy early and adhere to the prescribed exercises.
Q. How long does it take to recover from knee stiffness?
A. Recovery time varies, but most individuals experience significant improvement within 3-6 months. Severe cases may take longer, especially if surgery is required.
Q. Is surgery always necessary for knee stiffness?
A. Surgery is not always necessary. Many cases of post-operative stiffness improve with physical therapy, rest, and other non-invasive treatments.
Q. How can I prevent knee stiffness after knee replacement surgery?
A. Preventative measures include early and consistent physical therapy, avoiding prolonged immobility, and following your surgeon’s recommendations for activity restrictions and exercises.
Summary and Takeaway
Knee stiffness after knee replacement is a common issue that can significantly affect recovery and function. While most cases can be managed with physical therapy and non-surgical treatments, some patients may require surgical interventions like MUA or arthroscopic surgery. Early intervention and consistent rehabilitation are key to ensuring a successful recovery and preventing long-term complications.
Clinical Insight & Recent Findings
A recent study investigated the impact of prior knee surgeries on postoperative outcomes following knee replacement arthroplasty (KRA). The findings indicated that a history of previous knee surgery significantly increases the risk of complications such as prosthesis revision, infections, pain, and stiffness after total knee replacement (TKA).
Notably, patients with prior knee surgeries exhibited a 1.73-fold higher incidence of postoperative stiffness compared to those without a surgical history. This aligns with the understanding that previous surgeries, particularly those involving knee soft tissues or bones, contribute to fibrosis, joint adhesions, and altered knee mechanics, which complicate recovery and function after KRA.
The study emphasizes the need for enhanced preoperative assessment and targeted perioperative strategies for patients with a history of knee surgery to mitigate these risks. (“Study of prior knee surgery and complications after KRA – See PubMed”.)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons specializing in knee replacements are involved in diagnosing and managing post-surgical stiffness. Physical therapists and rehabilitation specialists play a key role in recovery.
When to See a Specialist?
Consult a specialist if knee stiffness persists despite rehabilitation or if it interferes with daily activities, especially if the knee is difficult to bend or straighten.
When to Go to the Emergency Room?
Go to the emergency room if you experience severe pain, swelling, or signs of infection following knee replacement surgery.
What Recovery Really Looks Like?
Recovery involves a combination of rest, physical therapy, and gradual reintroduction to activity. Most patients will regain full or nearly full range of motion after several months of rehabilitation.
What Happens If You Ignore It?
Ignoring stiffness after knee replacement can lead to chronic pain, limited mobility, and a decreased quality of life. Early treatment and rehabilitation are essential for preventing long-term complications.
How to Prevent It?
Prevent stiffness by adhering to prescribed physical therapy, avoiding prolonged immobility, and following your surgeon’s guidelines regarding activity levels after surgery.
Nutrition and Bone or Joint Health
A healthy diet rich in calcium and vitamin D supports bone health and joint recovery. Proper nutrition is essential for maintaining muscle strength and joint function after knee replacement.
Activity and Lifestyle Modifications
Engage in low-impact activities such as swimming or cycling during recovery and gradually increase activity levels as advised by your healthcare provider.
Do you have more questions?
What exactly causes scar tissue to form excessively after knee replacement surgery?
Excessive scar tissue can form due to a combination of the body’s natural healing process and factors such as the patient’s individual inflammatory response, prolonged immobility, or suboptimal surgical technique. Keeping the joint moving and ensuring proper alignment during surgery can help minimize this risk.
Are there specific risk factors that increase the likelihood of developing stiff TKA?
Yes, risk factors include advanced age, obesity, diabetes, smoking, and previous knee surgeries. Patients with inflammatory joint diseases like rheumatoid arthritis are also at higher risk.
How is the range of motion (ROM) measured clinically?
ROM is measured using a device called a goniometer, which assesses the degree of knee flexion and extension during physical examination.
What is considered a normal range of motion after knee replacement?
A normal range of motion after knee replacement is typically 0 degrees of extension to at least 115 degrees of flexion, though individual outcomes can vary.
Can stiffness resolve on its own without intervention?
In some mild cases, stiffness might improve with regular activity and exercises. However, persistent stiffness usually requires professional intervention
What are the first steps in treating stiffness after TKA if noticed early?
Early treatment typically involves physical therapy focused on mobility exercises, possibly combined with anti-inflammatory medications to reduce pain and facilitate movement.
How effective is manipulation under anesthesia, and what are the risks?
Manipulation under anesthesia is generally effective in improving ROM when conservative measures fail. Risks include fractures, ligament injuries, or increased pain, although these are rare.
When is surgical revision considered necessary?
Surgical revision is considered if both physical therapy and manipulation under anesthesia do not adequately improve ROM or if there are structural problems with the prosthesis itself.
Can changes in lifestyle improve outcomes after experiencing stiffness?
Yes, maintaining a healthy weight, staying active, and adhering to a regular stretching and strengthening routine can improve outcomes and possibly prevent worsening stiffness.
What long-term care is recommended for someone with stiff TKA?
Long-term care includes regular follow-up visits with the orthopedic surgeon, ongoing physical therapy as needed, and continuous monitoring of knee function.
Are there any alternative therapies for treating stiffness?
Some patients find relief through acupuncture, hydrotherapy, or massage, though these should complement, not replace, traditional treatments.
How soon after surgery can stiffness begin to develop?
Stiffness can begin to develop as early as a few weeks post-surgery, particularly if the knee is not mobilized early or adequately.
Is there a genetic predisposition to developing stiffness?
There is some evidence suggesting genetic factors might influence the healing process and scar tissue formation, though research is ongoing.
What advancements in surgical techniques have reduced the incidence of stiff TKA?
Advances include improved prosthetic designs, better precision in implant placement, and minimally invasive surgical techniques that preserve muscle and tissue integrity.
How does patient psychology affect recovery from stiff TKA?
Patient motivation and mental health significantly affect recovery. Depression or anxiety can hinder participation in rehabilitation and negatively impact outcomes.
What are the indicators that a revision surgery might be successful in resolving stiffness?
Good indicators include identifiable mechanical issues with the implant, localized scar tissue that can be removed, or correctable misalignments
Are certain types of knee implants less likely to cause stiffness?
Yes, implants that more closely mimic the natural knee mechanics and those designed for high flexion tend to have lower rates of stiffness.
What role does diet play in recovery from knee surgery and preventing stiffness?
A healthy diet rich in vitamins, minerals, and anti-inflammatory foods can promote healing and reduce inflammation, aiding in the recovery process.
Can stiffness after knee replacement be completely cured?
While it may not always be possible to completely restore the original range of motion, significant improvements can often be achieved through appropriate interventions.
What are the complications of untreated stiff TKA?
Untreated stiffness can lead to chronic pain, decreased mobility, and deterioration of muscle function around the knee. This can severely impact the patient’s ability to perform daily activities and may lead to further surgical interventions.
How can stiffness after knee replacement impact a patient’s mental health?
Limited mobility and chronic pain associated with stiffness can lead to frustration, anxiety, and depression, significantly impacting the patient’s overall well-being and quality of life.
Is stiffness more common in older adults?
Yes, older adults may be more prone to stiffness due to decreased tissue elasticity and slower recovery rates, as well as more common pre-existing conditions such as osteoarthritis.
How does the rehabilitation program differ for patients with stiff TKA compared to typical post-knee replacement patients?
Rehabilitation programs for stiff TKA often require more intensive physiotherapy focused on increasing range of motion. These programs may also be longer and more aggressive, involving more frequent sessions.
What preventive measures can be taken before knee replacement surgery to reduce the risk of stiffness?
Preoperative measures include optimizing the patient’s health through weight management, strengthening exercises, and controlling blood sugar levels in diabetic patients. Pre-surgical physiotherapy can also prepare the tissues and improve outcomes.
What should patients expect during the recovery period to minimize the risk of developing stiffness?
Patients should expect to actively participate in a rigorous physiotherapy regimen, adhere to pain management strategies, and keep regular follow-up appointments with their surgeon. Immediate postoperative mobilization, as guided by the healthcare team, is crucial to minimize stiffness.

