Knee pain following a posterior cruciate ligament (PCL) injury can disrupt daily life and, if left unaddressed, may lead to long-term issues. When pain is accompanied by swelling, instability, or difficulty walking, seeking medical attention is crucial. At Complete Orthopedics, our expert team is dedicated to diagnosing and treating PCL injuries, offering tailored treatment plans, including surgical solutions if necessary.
How Common It Is and Who Gets It? (Epidemiology)
PCL injuries are less common than the more frequently discussed anterior cruciate ligament (ACL) injuries. However, they can occur in both athletes and non-athletes due to traumatic events such as falls, motor vehicle accidents, or sports-related injuries. PCL injuries are more prevalent in contact sports such as football, soccer, and basketball, where high-impact collisions occur.
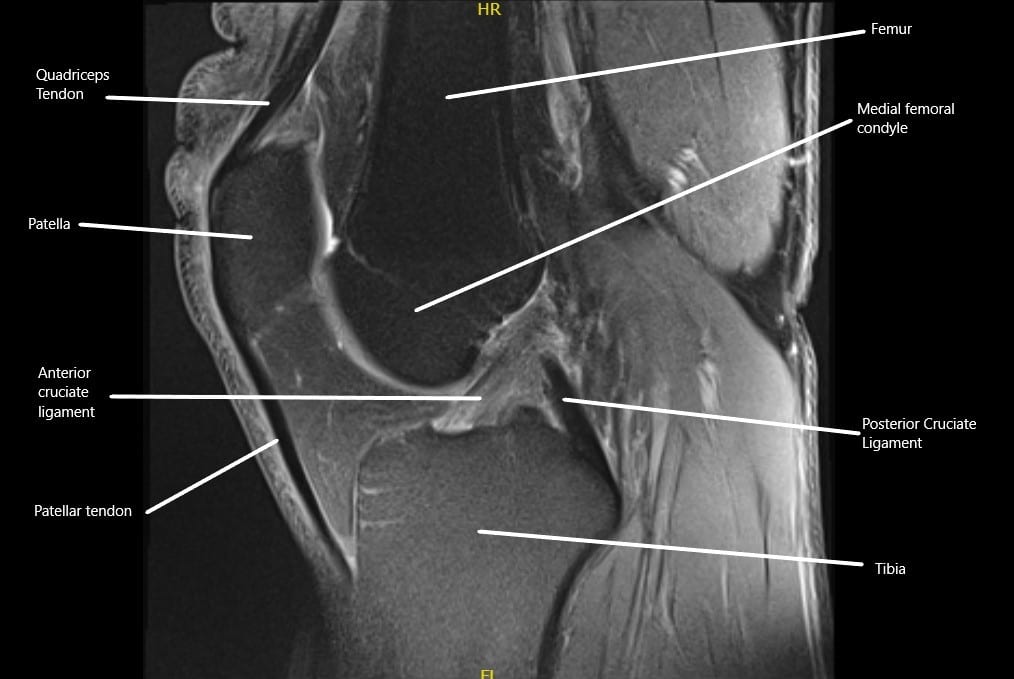
MRI showing the normal cruciate ligaments in the knee joint in the sagittal section.
Why It Happens – Causes (Etiology and Pathophysiology)
PCL injuries commonly occur from a direct trauma to the knee, such as falling onto a bent knee or a motor vehicle accident where the knee strikes the dashboard. Other causes include traumatic knee dislocations, rotational knee injuries, or sports accidents. The PCL helps stabilize the knee by preventing excessive backward movement of the shinbone (tibia) against the thigh bone (femur). Damage to the PCL compromises knee stability and function.
How the Body Part Normally Works? (Relevant Anatomy)
The posterior cruciate ligament (PCL) is located inside the knee joint, connecting the back of the femur (thigh bone) to the front of the tibia (shinbone). It stabilizes the knee by preventing the tibia from moving too far backward relative to the femur. The PCL works with the anterior cruciate ligament (ACL) and other supporting structures to ensure the knee remains stable during movement, especially when bending or rotating.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of a PCL injury vary depending on the severity of the tear. Acute injuries may cause immediate pain, swelling, and difficulty walking. A patient might feel a sense of knee instability or a sensation of the knee “giving away.” Chronic PCL injuries, however, might present with mild pain, instability, or difficulty performing specific movements, such as running or pivoting.
How Doctors Find the Problem? (Diagnosis and Imaging)
To diagnose a PCL injury, the physician will conduct a detailed physical examination and review the mechanism of injury. One common test is the posterior drawer test, where the doctor attempts to move the shinbone backward while the knee is bent, checking for excessive movement. X-rays are used to rule out bone fractures, while an MRI provides a clear image of the soft tissues, including the PCL, to confirm the extent of the injury.
Classification
PCL injuries are classified based on the degree of damage to the ligament:
- Grade 1: A mild sprain with some stretching of the ligament fibers.
- Grade 2: A partial tear of the ligament.
- Grade 3: A complete tear of the ligament, often requiring surgical intervention.
Other Problems That Can Feel Similar (Differential Diagnosis)
Other conditions that may present with similar symptoms include ACL injuries, meniscus tears, or general knee instability. A thorough examination and imaging studies are essential for differentiating between these conditions and accurately diagnosing a PCL injury.
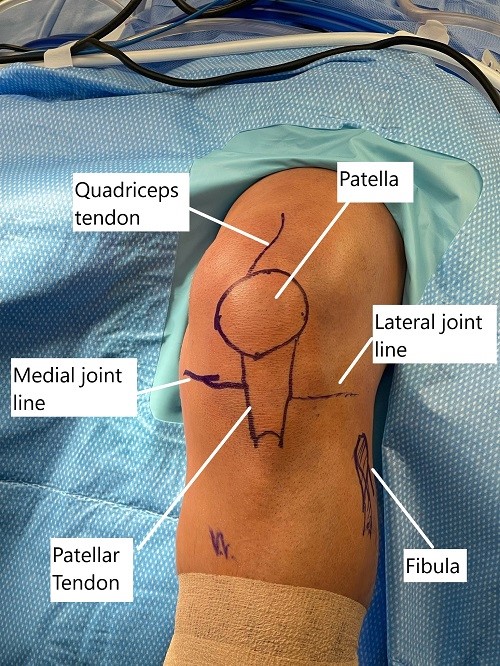
Intraoperative skin markings of the knee joint before arthroscopic reconstruction.
Treatment Options
Non-Surgical Care
For grade 1 and 2 PCL injuries, conservative treatment is often effective. This includes rest, ice therapy, compression, and elevation (R.I.C.E.) to reduce swelling and pain. Physical therapy plays a key role in strengthening the muscles around the knee, improving stability, and enhancing function. A knee brace may also be prescribed to provide support during the healing process.
Surgical Care
If conservative treatments are unsuccessful or in the case of grade 3 or 4 injuries, surgery is often required. Surgical reconstruction of the PCL is performed using either an autograft (tissue taken from the patient’s own body) or an allograft (tissue from a donor). Common donor sites for autografts include the hamstrings tendon, Achilles tendon, or quadriceps tendon. Surgery is typically done arthroscopically, allowing for minimal incisions and faster recovery.
Recovery and What to Expect After Treatment
The recovery process for PCL injuries depends on the severity of the injury and the treatment approach. Non-surgical treatment may require several weeks of rehabilitation to regain knee strength and stability. Post-surgical recovery can take several months, with a gradual increase in activity under the guidance of a rehabilitation specialist. Physical therapy is essential to improve mobility and strength in the knee.
Possible Risks or Side Effects (Complications)
As with any surgery, PCL reconstruction carries risks, including infection, blood clots, or damage to surrounding structures. The rehabilitation process may also lead to muscle stiffness or weakness if not followed correctly. In some cases, the reconstructed ligament may not fully heal, necessitating further intervention.
Long-Term Outlook (Prognosis)
With proper treatment, most individuals recover well from PCL injuries. Non-surgical treatments for mild injuries usually result in a full recovery with no long-term issues. Surgical outcomes are generally favorable, though full recovery from surgery can take several months, and patients may experience occasional knee instability if the ligament does not heal properly.
Out-of-Pocket Costs
Medicare
CPT Code 29889 – PCL Reconstruction (Arthroscopic/Open): $290.95
CPT Code 27560 – PCL Repair (Primary Repair): $91.42
CPT Code 27428 – PCL Reconstruction With Graft: $266.00
Under Medicare, 80% of the approved amount for these procedures is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, leaving most patients with little to no out-of-pocket expenses for Medicare-approved knee surgeries. These supplemental plans work directly with Medicare to ensure full coverage for the procedures.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, ranging from $100 to $300, depending on the specific policy and network status.
Workers’ Compensation
If your knee surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your knee injury resulting in surgery is caused by a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses, including PCL repair and reconstruction procedures. The only possible out-of-pocket cost may be a small deductible depending on your individual policy terms.
Example
James, a 45-year-old patient with a torn posterior cruciate ligament, required PCL reconstruction with graft (CPT 27428). His estimated Medicare out-of-pocket cost was $266.00. Since James had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. What causes a posterior cruciate ligament injury?
A. PCL injuries typically occur due to trauma, such as falling on a bent knee, motor vehicle accidents, or sports injuries.
Q. Can a PCL injury heal without surgery?
A. Yes, grade 1 and 2 PCL injuries often heal with conservative treatments like rest, ice, and physical therapy.
Q. How long does it take to recover from a PCL injury?
A. Recovery time varies. Non-surgical treatment may take several weeks, while surgical recovery may take several months, depending on rehabilitation progress.
Q. What are the signs that I need surgery for a PCL injury?
A. If your symptoms persist or worsen despite non-surgical treatment, or if you have a complete tear (grade 3 injury), surgery may be necessary.
Q. Will I be able to return to sports after a PCL injury?
A. Most patients return to sports after PCL injury treatment, but this depends on the severity of the injury and adherence to rehabilitation protocols.
Summary and Takeaway
Posterior cruciate ligament injuries are less common than ACL injuries but can significantly impact knee function and mobility. Treatment depends on the severity of the injury, with non-surgical management for mild injuries and surgery for more severe cases. Proper rehabilitation is key to recovery, and most patients can return to normal activities with time and effort.
Clinical Insight & Recent Findings
A recent study evaluated long-term outcomes of non-operative management for acute posterior cruciate ligament (PCL) injuries using a physiotherapy-led exercise and support brace intervention.
The results demonstrated significant improvements in patient-reported outcomes, including the International Knee Documentation Committee (IKDC) score, Knee injury and Osteoarthritis Outcome Score (KOOS), and Tegner Activity Scale (TAS), five years after injury. Notably, only 14% of patients required surgical reconstruction, with the need for surgery being most common within the first two years.
These findings suggest that a structured rehabilitation approach can be highly effective in managing acute PCL injuries, with low conversion rates to surgical intervention. (“Study on Non-Operative Treatment of PCL Injuries – see PubMed”).
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons specializing in sports medicine or knee surgeries typically perform PCL injury treatment, with a team that may include physical therapists and rehabilitation specialists.
When to See a Specialist?
Consult a specialist if you experience knee pain, instability, or difficulty walking after a trauma or injury, especially if symptoms do not improve with rest and physical therapy.
When to Go to the Emergency Room?
Go to the emergency room if you experience severe pain, swelling, or inability to move the knee, especially following an acute injury, as this may indicate a more severe tear or fracture.
What Recovery Really Looks Like?
Recovery from a PCL injury involves a combination of rest, rehabilitation, and gradual return to activities. Full recovery may take several months, and adherence to rehabilitation protocols is essential for regaining knee strength and stability.
What Happens If You Ignore It?
Ignoring a PCL injury can lead to chronic knee instability, increased wear on the knee joint, and the risk of further ligament or meniscus damage. Early treatment is key to preventing long-term complications.
How to Prevent It?
While some PCL injuries are unavoidable, wearing protective gear during sports, strengthening the muscles around the knee, and practicing proper techniques during physical activities can help reduce the risk.
Nutrition and Bone or Joint Health
A balanced diet rich in calcium and vitamin D supports bone health and can aid in recovery after a PCL injury. Maintaining a healthy weight can also reduce stress on the knee joint.
Activity and Lifestyle Modifications
To prevent further injury, engage in low-impact activities such as swimming or cycling during recovery. Follow your surgeon’s guidelines regarding activity levels, and avoid high-impact activities until your knee is fully rehabilitated.
Do you have more questions?
What are the long-term effects of a PCL injury if left untreated?
Long-term effects can include chronic knee instability, pain, decreased function, and a higher risk of developing osteoarthritis.
How can PCL injuries be prevented, especially in athletes?
Prevention strategies include strengthening knee muscles, improving flexibility, using proper sports techniques, wearing appropriate footwear, and using knee braces during high-risk activities.
Are there any new treatments on the horizon for PCL injuries?
Research is ongoing into more advanced surgical techniques and materials for ligament reconstruction, as well as the use of biologics like platelet-rich plasma (PRP) and stem cells to enhance healing.
How does age affect the treatment and recovery of a PCL injury?
Younger individuals generally recover faster and more completely due to better tissue healing capacity. Treatment plans may vary based on age, with more conservative treatments considered for older adults.
Is a brace necessary for PCL injury recovery?
A brace can be helpful in stabilizing the knee during the initial recovery phase, especially for severe injuries. It supports the knee as it heals and can help prevent further injury during physical therapy.
How soon can one return to sports after a PCL injury?
Returning to sports depends on the severity of the injury and the individual’s progress in rehabilitation. It typically ranges from several months to a year, ensuring the knee has regained sufficient strength and stability
What is the success rate of PCL surgery?
The success rate for PCL surgery is generally high, with many patients returning to their pre-injury level of activity. Success depends on the surgical technique, the severity of the injury, and adherence to post-surgery rehabilitation.
Are there any alternative therapies for PCL injuries?
Alternative therapies might include acupuncture, massage, and specific exercises that focus on strengthening the muscles around the knee to compensate for the injured ligament.
Can a PCL injury recur after treatment?
Recurrence is uncommon if the injury is properly managed with appropriate rehabilitation and if activities that might cause reinjury are avoided or approached with caution.
What lifestyle changes might be recommended post-PCL injury?
Lifestyle changes may include maintaining a healthy weight to reduce stress on the knee, avoiding activities that involve heavy impact or sudden changes in direction, and incorporating low-impact exercises like swimming or cycling into one’s routine.
Where is the posterior cruciate ligament located?
Posterior cruciate ligament is located inside the knee and it attaches the lower end of femur to the upper end of tibia. It courses from the top and in the front to lower down on the back side of the upper end of tibia. It is present behind the anterior cruciate ligament.
What the symptoms of posterior cruciate ligament injury?
Posterior cruciate ligament injury usually happens due to fall or accident. These patients usually present with pain and swelling of the knee and may have instability. They may also complain of hearing a pop at the time of injury.
Can a torn PCL heal on its own?
The patients who have partial tearing of the PCL may heal by themselves. These patients are usually treated with brace and physical therapy and are re-evaluated to look for optimal healing of the PCL. If the tearing of the PCL is high grade or complete, then these patients may need reconstruction or repair of the PCL.
What is the surgery for PCL injury?
The patients who have high grade tearing or complete tear of the PCL may need repair or reconstruction of the PCL. In cases of repair, the PCL is fixed back to the bone with use of sutures and anchors. In case the patient needs reconstruction, then the PCL is reconstructed using tendons either from the patient’s body or from cadaveric origin to reconstruct the PCL using sutures and anchors or buttons.
How long does it take to recover from a torn PCL?
The patients who have partial tearing of the PCL may take two to four months of physical therapy and rehabilitation to recover completely from the PCL injury. The patients who have undergone surgery for the torn PCL may take 6 to 12 months to completely recover and get back to the preinjury status of activity or sportsmanship.
What is the function of posterior cruciate ligament?
The posterior cruciate ligament provides stability to the knee joint. It works in concordance with other ligaments of the knee, including the anterior cruciate ligament, the medial collateral ligament, lateral collateral ligament and the capsule to keep the knee stable during daily activities as well as sports.
Do all PCL tears require surgery?
Low grade PCL tears can be treated conservatively with the use of brace and physical therapy. Patients with high grade PCL tear or complete tearing of the PCL may require surgery in the form of repair or reconstruction of the ligament.

