Iliotibial Band Syndrome (ITBS) is a common condition that causes pain on the outside of the knee. It is particularly prevalent in individuals who engage in activities that involve repetitive knee movements, such as running, cycling, or other athletic pursuits. The condition arises from the inflammation of the iliotibial band (ITB), a thick band of tissue that runs along the outer side of the leg. While ITBS is typically an overuse injury, it can also be exacerbated by factors such as poor biomechanics, inadequate footwear, or training errors. This article aims to provide a comprehensive overview of ITBS, from its causes and symptoms to treatment and prevention strategies.
How Common It Is and Who Gets It? (Epidemiology)
ITBS is most commonly seen in athletes, particularly runners and cyclists. It tends to affect individuals who participate in repetitive physical activities involving excessive knee bending and straightening. Although ITBS is common among athletes, it can also occur in individuals with poor biomechanics, muscle imbalances, or improper footwear. The condition is more frequent in individuals who suddenly increase the intensity or duration of their training.
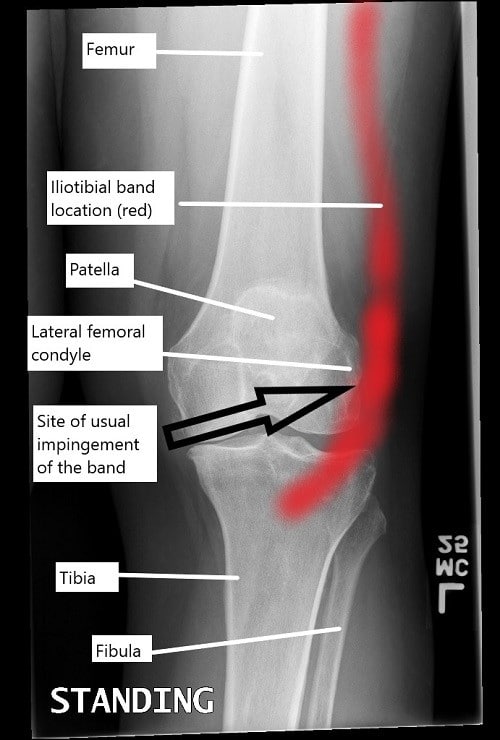
A knee x-ray illustrating the location of iliotibial band and the usual site of impingement.
Why It Happens – Causes (Etiology and Pathophysiology)
ITBS occurs when the iliotibial band, a thick band of connective tissue running from the hip to the shin, becomes irritated and inflamed. The most common causes of ITBS include:
- Overuse: Repetitive knee movements, such as running or cycling, can cause the ITB to rub against the lateral femoral condyle (the outer part of the knee), leading to inflammation.
- Poor Biomechanics: Issues like improper foot alignment, weak hip muscles, or poor posture during physical activities can increase stress on the ITB, leading to irritation.
- Training Errors: Sudden increases in activity intensity or duration without proper rest can overload the ITB.
- Improper Equipment: Worn-out shoes or inadequate support from sports equipment can exacerbate the symptoms of ITBS.
How the Body Part Normally Works? (Relevant Anatomy)
The iliotibial band is a fibrous band that runs along the outer side of the thigh, extending from the hip to the shinbone. It connects the tensor fascia lata and gluteus maximus muscles to the tibia. The ITB helps stabilize the knee during activities such as walking, running, and cycling. Normally, the ITB moves smoothly over the lateral femoral condyle as the knee bends and straightens. However, when the ITB becomes tight or irritated, it can rub against the femoral condyle, leading to inflammation and pain.
What You Might Feel – Symptoms (Clinical Presentation)
The primary symptom of ITBS is pain on the outer side of the knee, which worsens with activities such as running, cycling, or descending stairs. Other common symptoms include:
- Swelling or tenderness on the outside of the knee.
- Pain that worsens when going downhill or downstairs, or with repetitive leg movements.
- A popping or snapping sensation over the outer knee, especially when bending or straightening the leg.
- Stiffness and limited range of motion in the knee.
- Instability or a feeling of weakness in the knee, especially during physical activities.
- Grinding or clicking sounds when the knee moves.
How Doctors Find the Problem? (Diagnosis and Imaging)
A diagnosis of ITBS typically begins with a thorough physical examination, during which the physician will assess the knee for signs of tightness, inflammation, and pain. Specific tests used to diagnose ITBS include:
- Ober’s Test: The patient lies on their side, and the examiner moves the leg to check for tightness of the iliotibial band. A positive test occurs if the thigh cannot move past the body’s midline.
- Noble Compression Test: The physician applies pressure to the outside of the knee while bending and straightening the leg. Pain at a 30-40 degree angle of knee flexion is considered positive.
- Imaging: An MRI or ultrasound may be ordered to rule out other conditions, such as ligament or meniscus injuries, or to check for inflammation in the ITB.
Classification
ITBS is typically classified based on the severity of symptoms and their impact on daily activities:
- Grade 1: Mild pain that occurs after physical activity but resolves with rest.
- Grade 2: Moderate pain that persists during and after activity but does not significantly affect daily functions.
- Grade 3: Severe pain that occurs during normal activities and limits the ability to perform sports or daily tasks.
Other Problems That Can Feel Similar (Differential Diagnosis)
Several conditions may cause symptoms similar to ITBS, including:
- Meniscal Tears: Tears in the cartilage of the knee may cause pain, swelling, and mechanical symptoms like clicking or locking.
- Patellofemoral Stress Syndrome: Pain around the kneecap, often due to maltracking or overuse, can mimic the symptoms of ITBS.
- Lateral Collateral Ligament (LCL) Injury: Injury to the ligament on the outer side of the knee can cause pain, instability, and swelling similar to ITBS.
- Bursitis: Inflammation of the bursa (fluid-filled sacs) around the knee joint may cause pain on the outer knee, which can be mistaken for ITBS.
Treatment Options
Non-Surgical Care
Most cases of ITBS can be managed with non-surgical treatments:
- Rest and Activity Modification: Reducing or altering activities that aggravate the ITB, such as running or cycling, is essential for recovery. Low-impact activities like swimming or yoga can help maintain fitness while allowing the knee to heal.
- Ice Therapy: Applying ice to the outside of the knee for 15-20 minutes several times a day can reduce inflammation and alleviate pain.
- NSAIDs: Over-the-counter anti-inflammatory medications, such as ibuprofen, can help reduce pain and swelling.
- Physical Therapy: A physical therapist can guide exercises to stretch the ITB and strengthen the hip abductor muscles, which can improve stability and relieve tension on the ITB.
- Ultrasound Therapy: In some cases, ultrasound therapy may be used to reduce inflammation and improve healing in the affected area.
Surgical Care
Surgical treatment is rare and is generally considered only when conservative treatments fail:
- ITB Release Surgery: In cases where the ITB remains tight and resistant to conservative treatment, a small section of the band may be surgically released to relieve tension and prevent further irritation.
- Arthroscopic Surgery: In rare cases, arthroscopy may be used to remove scar tissue or debris that is causing impingement of the ITB.
Recovery and What to Expect After Treatment
Recovery from ITBS generally involves rest, rehabilitation, and gradual return to activity:
- Initial Recovery: After beginning treatment, you may need to rest and avoid activities that aggravate the knee. Ice therapy and medications can help manage inflammation and pain.
- Physical Therapy: A physical therapist will help you perform targeted exercises to improve flexibility, strengthen muscles, and restore knee function. This phase typically lasts several weeks to months.
- Gradual Return to Activity: As symptoms improve, activities like running and cycling can be reintroduced gradually, starting with lower intensities and durations.
- Long-Term Care: Continued strengthening and stretching exercises can help prevent recurrence of ITBS.
Recovery
Step 1:
Rest and Activity Modification: The first step in recovering from ITBS is giving your knee time to heal. This means avoiding activities that worsen your symptoms, such as running or cycling, and opting for low-impact exercises like swimming or yoga instead. Rest doesn’t mean complete inactivity; it’s about finding a balance that allows your body to recover while staying active in ways that don’t aggravate your knee.
Step 2:
Ice Therapy: Applying ice packs to the affected area can help reduce inflammation and alleviate pain. Ice therapy is most effective when applied for 15-20 minutes several times a day, especially after activities that may strain your knee.
Step 3:
Stretching and Strengthening Exercises: Physical therapy plays a crucial role in ITBS recovery, focusing on stretching and strengthening exercises to improve flexibility and stability around the knee. Simple stretches targeting the ITB and surrounding muscles, such as the hip flexors and quadriceps, can help alleviate tightness and reduce strain on the knee.
Step 4
Foam Rolling: Foam rolling is another effective way to massage the ITB and surrounding muscles, releasing tension and promoting blood flow to the affected area. Using a foam roller regularly can help prevent stiffness and improve mobility as you progress through your recovery.
Step 5:
Gradual Return to Activity: As your symptoms improve, gradually reintroduce activities that may have caused discomfort in the past. Start with shorter durations and lower intensities, gradually increasing as your knee tolerates. Listen to your body and avoid pushing through pain, as this can delay your recovery or lead to setbacks.
Possible Risks or Side Effects (Complications)
Complications from ITBS treatment are rare but can include:
- Infection: Although uncommon, surgical treatments like ITB release can carry a small risk of infection.
- Reinjury: Returning to activity too soon or without adequate rehabilitation can lead to reinjury.
- Stiffness: In rare cases, surgery or prolonged rest can result in joint stiffness or loss of range of motion.
Long-Term Outlook (Prognosis)
Most patients with ITBS recover fully with conservative treatment. Recovery time varies, but with proper care, patients can typically return to their activities within a few weeks to months. Surgical treatments are effective but are rarely necessary, and most patients experience relief with physical therapy and activity modifications.
Out-of-Pocket Cost
Medicare
CPT Code 27305 – ITB Release Surgery (Open IT Band Release): $116.25
Under Medicare, 80% of the approved amount for this procedure is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, leaving most patients with little to no out-of-pocket expenses for Medicare-approved ITB release surgeries. These supplemental plans coordinate directly with Medicare to provide full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or any uncovered charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on the specific policy and network status.
Workers’ Compensation
If your ITB release surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your ITB release surgery is the result of a motor vehicle accident, No-Fault Insurance will cover the full cost of the procedure. The only possible out-of-pocket cost may be a small deductible depending on your individual policy terms.
Example
Chris, a 45-year-old patient with iliotibial band syndrome, underwent open ITB release surgery (CPT 27305). His estimated Medicare out-of-pocket cost was $116.25. Since Chris had supplemental insurance through AARP Medigap, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. What causes Iliotibial Band Syndrome?
A. ITBS is primarily caused by overuse, improper biomechanics, and muscle imbalances, often due to repetitive knee movements like running or cycling.
Q. How is ITBS treated?
A. Treatment for ITBS includes rest, ice therapy, physical therapy, NSAIDs, and in rare cases, surgery to release the ITB.
Q. Can ITBS be prevented?
A. ITBS can be prevented by gradually increasing training intensity, using proper equipment, incorporating cross-training, and performing regular stretching and strengthening exercises.
Summary and Takeaway
Iliotibial Band Syndrome is a common condition, especially among athletes, that can cause pain and discomfort on the outer side of the knee. With appropriate treatment, such as physical therapy, rest, and activity modification, most patients recover fully. If symptoms persist, surgical options may be considered. Proper care, including gradual increases in activity and appropriate equipment, can help prevent ITBS from recurring.
Clinical Insight & Recent Findings
A recent study systematically reviewed the effectiveness of conservative treatment strategies for iliotibial band syndrome (ITBS) in runners, focusing on pain relief and functional outcomes.
The study found that hip abductor strengthening (HAS) exercises were consistently beneficial across various treatment approaches, both as a standalone and combined therapy. Combined treatment strategies, including HAS with shockwave therapy or manual therapy, showed significant improvements in pain and function.
Notably, HAS exercises, especially when integrated with gait retraining, were linked to improved outcomes in both pain reduction and functional recovery. The review suggests that a multimodal approach is more effective for managing ITBS than single interventions. (“Study of conservative treatments for ITBS – See PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons, physical therapists, and sports medicine specialists are the primary healthcare providers involved in diagnosing and treating ITBS.
When to See a Specialist?
If you experience persistent pain on the outer knee that doesn’t improve with rest, or if the pain interferes with daily activities, it’s important to consult a specialist for evaluation and treatment.
When to Go to the Emergency Room?
Seek emergency care if you experience severe pain, significant swelling, or signs of infection (e.g., warmth, redness) in the knee.
What Recovery Really Looks Like?
Recovery typically involves physical therapy, gradual return to activity, and lifestyle adjustments to prevent further strain on the knee.
What Happens If You Ignore It?
Ignoring ITBS can lead to chronic pain, reduced mobility, and possible long-term damage to the knee joint. Early intervention is key to a full recovery.
How to Prevent It?
Prevent ITBS by gradually increasing physical activity, using proper footwear, and performing strengthening and stretching exercises to support the knee and hip muscles.
Nutrition and Bone or Joint Health
Maintain a balanced diet rich in vitamins and minerals, including calcium and vitamin D, to support joint health and reduce the risk of injury.
Activity and Lifestyle Modifications
Incorporate low-impact activities like swimming or cycling into your routine to reduce stress on the knee joint and help prevent overuse injuries.
Do you have more questions?
What are the long-term consequences of untreated ITBS?
Untreated ITBS can lead to chronic knee pain and instability, potentially interfering with daily activities and reducing quality of life. It may also increase the risk of developing other knee-related conditions, such as patellofemoral pain syndrome or osteoarthritis, in the long term.
Can ITBS affect other parts of the body besides the knee?
While ITBS primarily affects the knee, it can also cause compensatory changes in gait and posture, leading to secondary issues such as hip pain, lower back pain, or foot problems.
Is surgery ever necessary to treat ITBS?
In rare cases where conservative treatments fail to provide relief, surgical intervention may be considered. Procedures such as ITB release or bursectomy may be performed to alleviate persistent symptoms and restore function.
How soon can I return to physical activity after experiencing ITBS symptoms?
The timeline for returning to physical activity varies depending on the severity of symptoms and individual healing rates. It’s crucial to gradually reintroduce activities once symptoms have resolved and to listen to your body to avoid exacerbating the condition.
Are there any specific stretches or exercises I should avoid if I have ITBS?
While stretching and strengthening exercises are generally beneficial for managing ITBS, certain movements that place excessive stress on the ITB, such as deep lunges or leg presses with heavy weights, may exacerbate symptoms and should be approached with caution.
Can ITBS occur in both knees simultaneously?
Yes, ITBS can affect both knees simultaneously, especially in cases where underlying biomechanical issues or training errors are present bilaterally. Symmetrical symptoms in both knees may indicate a systemic problem that requires comprehensive evaluation and treatment.
Are there any dietary supplements or medications that can help alleviate ITBS symptoms?
While there is limited scientific evidence supporting the use of dietary supplements or medications specifically for ITBS, anti-inflammatory medications such as ibuprofen may help reduce pain and inflammation in the short term. However, it’s essential to consult with a healthcare professional before starting any new supplements or medications.
Can ITBS be prevented through specific warm-up routines?
While warming up before physical activity can help prepare the muscles and joints for exercise, there is limited evidence to suggest that specific warm-up routines can prevent ITBS outright. However, incorporating dynamic stretches and activation exercises targeting the hip and knee muscles may help reduce the risk of injury.
Is ITBS more common in a particular age group?
While ITBS can occur in individuals of all ages, it is more commonly seen in younger athletes, particularly those engaged in activities such as running, cycling, or sports that involve repetitive knee movement.
How can I differentiate between ITBS and other knee conditions with similar symptoms?
Diagnosing ITBS typically involves a thorough physical examination and may require imaging tests to rule out other potential causes of knee pain, such as patellofemoral pain syndrome, meniscal injury, or iliotibial band friction syndrome.
Can wearing a knee brace help alleviate ITBS symptoms?
While knee braces may provide temporary relief by stabilizing the knee joint and reducing strain on the ITB, they are not typically considered a long-term solution for managing ITBS. Physical therapy and biomechanical corrections are generally more effective in addressing the underlying causes of ITBS.
Are there any specific risk factors that increase the likelihood of developing ITBS?
Several factors, including training errors, biomechanical abnormalities, muscle imbalances, and improper footwear, can increase the risk of developing ITBS. Individuals with a history of previous knee injuries or those with excessive foot pronation may also be more predisposed to ITBS.
Can ITBS occur suddenly, or is it typically a gradual onset?
ITBS can occur both suddenly and gradually, depending on the underlying cause and individual factors. While sudden onset ITBS may be triggered by a specific incident or activity, gradual onset ITBS often develops over time due to repetitive stress or overuse.
Is it possible to completely recover from ITBS?
With appropriate treatment and rehabilitation, many individuals can fully recover from ITBS and return to their previous level of activity. However, it’s essential to address underlying biomechanical issues and adopt preventive measures to reduce the risk of recurrence.
Can wearing orthotic inserts in my shoes help prevent ITBS?
Orthotic inserts may help correct biomechanical abnormalities and provide additional support and cushioning, reducing the risk of ITBS in some individuals. However, they should be prescribed and fitted by a qualified healthcare professional based on individual needs and foot mechanics.
Are there any specific activities I should avoid if I have ITBS?
Activities that exacerbate ITBS symptoms, such as running downhill or on uneven surfaces, should be avoided until symptoms have resolved. It’s essential to listen to your body and modify activities accordingly to prevent further irritation of the ITB.
Can ITBS lead to permanent damage to the knee joint?
In severe or chronic cases, untreated ITBS may contribute to structural changes in the knee joint, such as cartilage degeneration or patellar malalignment, which could potentially lead to long-term complications if left unaddressed.
Is there a genetic predisposition to developing ITBS?
While genetic factors may play a role in predisposing individuals to certain biomechanical abnormalities or musculoskeletal conditions that contribute to ITBS, the condition is primarily attributed to external factors such as training errors and overuse.
Can ITBS be exacerbated by changes in weather or environmental conditions?
While there is limited scientific evidence linking changes in weather or environmental conditions directly to ITBS exacerbations, factors such as temperature extremes, humidity, or terrain may indirectly impact symptoms by affecting joint lubrication and muscle performance.
How long does it typically take to recover from ITBS with conservative treatments?
The recovery time for ITBS varies depending on the severity of symptoms, individual healing rates, and adherence to treatment recommendations. With conservative treatments such as rest, physical therapy, and activity modification, many individuals experience improvement within a few weeks to a few months.
Are there any specific strategies for managing ITBS during athletic competitions or events?
During athletic competitions or events, managing ITBS involves a combination of proper warm-up and cool-down routines, pacing strategies to avoid overexertion, and using supportive taping or bracing techniques to minimize stress on the ITB and knee joint.
Can ITBS recur even after successful treatment?
Yes, ITBS can recur, especially if underlying biomechanical issues or training errors are not addressed adequately. Implementing preventive measures such as cross-training, proper footwear, and ongoing maintenance exercises can help reduce the risk of recurrence.

