After knee replacement surgery, some patients may experience a clunking sensation in their knee when straightening or bending it. This symptom, often concerning, can be associated with a condition known as Patellar Clunk Syndrome. This condition results from the formation of fibrous tissue near the patella (kneecap) and is most commonly seen in patients who have undergone posterior stabilized knee replacement. While rare, this issue is manageable with the appropriate treatment, and understanding its causes, symptoms, and treatment options is essential for those affected.
How Common It Is and Who Gets It? (Epidemiology)
Clunking after knee replacement is a relatively uncommon complication, more frequently seen in patients with posterior stabilized implants, which were more common in older prosthetic designs. It primarily affects patients who underwent TKR using these older implant models, though the incidence has decreased with the advent of newer designs. It can occur in any patient post-surgery, but it is more likely in those with issues such as a low-lying patella, improper prosthetic alignment, or a history of scar tissue formation in the knee.
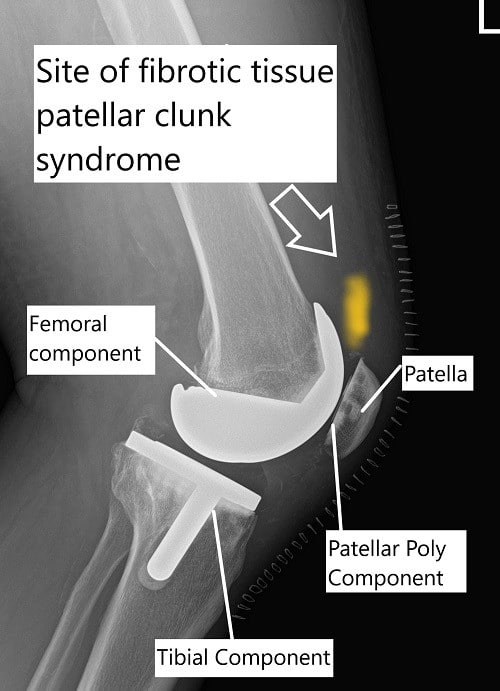
X-ray showing total knee replacement and the site of fibrous tissue in patellar clunk syndrome.
Why It Happens – Causes (Etiology and Pathophysiology)
Patellar Clunk Syndrome occurs due to the formation of fibrous tissue, or a fibrous nodule, on the undersurface of the patella. This fibrous tissue can get caught in the box-shaped femoral component of the knee prosthesis during movement, especially in posterior stabilized designs. Factors contributing to the development of this syndrome include:
- Direct Injury to the Quadriceps Muscle: During surgery, the quadriceps muscle, which is attached to the patella, may be disturbed, leading to the formation of scar tissue.
- Small Patellar Component: A patellar component that is too small or low in placement can increase the likelihood of fibrous tissue formation under the patella.
- Posterior Stabilized Implants: These implants have a mechanism that includes a femoral cam and tibial post, which, in combination with fibrous tissue, can cause a clunking sensation when the patella moves over the femoral component.
- Trauma or Pre-existing Fibrous Tissue: Pre-existing fibrous tissue from prior surgeries or knee conditions may also contribute to the syndrome.
How the Body Part Normally Works? (Relevant Anatomy)
The knee joint consists of three bones: the femur (thigh bone), tibia (shin bone), and the patella (kneecap). The femur and tibia are covered with articular cartilage to reduce friction, while the patella helps in smooth knee movements. The quadriceps muscle, which is attached to the patella, allows for extension of the knee. During knee replacement surgery, the damaged parts of the joint are replaced with prosthetic components, and the patella is typically resurfaced with a high-grade polyethylene insert to ensure smooth movement.
What You Might Feel – Symptoms (Clinical Presentation)
The primary symptom of Patellar Clunk Syndrome is a clunking or clicking sensation in the knee, which occurs when straightening or bending the knee. Other potential symptoms include:
- Pain: Pain or discomfort in the knee, especially when straightening the leg.
- Swelling: Some patients may experience swelling around the knee joint.
- Stiffness: A feeling of tightness or limited movement, particularly with flexion and extension of the knee.
- Instability: A sensation of the knee “giving way” or feeling unstable, especially during weight-bearing activities.
- Audible Sounds: The clunking sensation may also be accompanied by other sounds like clicking or popping as the knee moves.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis typically begins with a physical examination and an assessment of symptoms. Imaging tests may include:
- X-rays: To assess the alignment of the knee prosthesis and rule out issues like implant loosening or malposition.
- MRI: Used to examine soft tissue and the condition of the fibrous nodule or scar tissue.
- Arthroscopy: A minimally invasive procedure where a small camera is inserted into the knee joint, allowing the surgeon to directly visualize the source of the clunking and remove any scar tissue or loose bodies causing the issue.
Classification
Patellar Clunk Syndrome is classified based on the severity and nature of the clunking or catching:
- Mild: Intermittent clunking or clicking, generally without significant pain or functional limitations.
- Moderate: Clunking with some pain, limited motion, and occasional instability.
- Severe: Persistent clunking, pain, instability, and reduced knee function that may require surgical intervention.
Other Problems That Can Feel Similar (Differential Diagnosis)
Several conditions can cause symptoms similar to Patellar Clunk Syndrome, including:
- Implant Loosening: Loosening of the knee implant components can cause pain, instability, and abnormal joint movement.
- Meniscal Tears: Tears in the menisci can cause similar mechanical symptoms like clicking and locking.
- Ligament Issues: Instability or problems with ligaments like the ACL or PCL can also lead to knee buckling or a clunking sensation.
- Infection: Infections may cause swelling, warmth, and mechanical symptoms in the knee joint.
Treatment Options
Non-Surgical Care
- Physical Therapy: Strengthening the muscles around the knee and improving joint mechanics can help reduce clunking and discomfort.
- Pain Management: Over-the-counter pain medications, such as NSAIDs, may help manage symptoms, especially if there is associated pain or inflammation.
- Bracing: Knee braces can provide additional support, particularly if the clunking is related to instability or maltracking of the patella.
Surgical Care
If conservative measures do not resolve the issue, surgical intervention may be necessary:
- Arthroscopic Surgery: This minimally invasive procedure can be used to remove fibrous tissue or loose bodies from the knee joint that are causing the clunking.
- Revision Surgery: In more severe cases, a revision of the knee replacement may be required, especially if the implant is misaligned or the patella component is poorly positioned.
- Patellar Component Modification: If the clunking is due to a poorly positioned or undersized patellar component, it may be replaced or repositioned during revision surgery.
Recovery and What to Expect After Treatment
Recovery depends on the treatment approach:
- Post-Surgical Care: After arthroscopic surgery or revision, patients typically follow a rehabilitation plan to regain knee strength, mobility, and function. Physical therapy is often required to restore full movement.
- Recovery Timeline: Most patients recover within 4-6 weeks after arthroscopic surgery, although full rehabilitation may take several months.
Possible Risks or Side Effects (Complications)
Complications associated with treatment for Patellar Clunk Syndrome include:
- Infection: Any surgical procedure carries the risk of infection, which may require further treatment.
- Blood Clots: Blood thinners are often prescribed after surgery to prevent deep vein thrombosis (DVT).
- Implant Loosening: Even after revision surgery, there is still a risk of the implant loosening over time, especially in younger, more active patients.
- Knee Stiffness: Post-surgical stiffness or swelling can sometimes persist and may require ongoing physical therapy.
Long-Term Outlook (Prognosis)
The prognosis for Patellar Clunk Syndrome is generally favorable, especially with early intervention. Most patients experience relief from the clunking sensation and pain with appropriate treatment, whether it’s physical therapy, arthroscopic surgery, or implant adjustment. The success rate of revision surgeries is high, but long-term outcomes depend on factors like age, activity level, and the severity of the symptoms.
Out-of-Pocket Costs
Medicare
CPT Code 29877 – Arthroscopic Surgery (Debridement/Loose Body Removal): $148.26
CPT Code 29874 – Arthroscopic Surgery (Loose Body Removal): $127.98
CPT Code 27487 – Revision Total Knee Replacement (Femoral + Tibial Components): $413.16
CPT Code 27486 – Patellar Component Revision: $332.04
Under Medicare, 80% of the approved amount for these procedures is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved knee surgeries and arthroscopic procedures. These supplemental plans work directly with Medicare to ensure full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it functions as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, ranging from $100 to $300, depending on the specific policy and network status.
Workers’ Compensation
If your knee surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your knee injury resulting in surgery is the result of a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses. The only possible out-of-pocket cost may be a small deductible depending on your individual policy terms.
Example
Michael, a 58-year-old patient with knee arthritis, required arthroscopic surgery (CPT 29877) for loose body removal and a revision total knee replacement (CPT 27487). His estimated Medicare out-of-pocket costs were $148.26 for the arthroscopy and $413.16 for the knee replacement revision. Since Michael had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for the procedures.
Frequently Asked Questions (FAQ)
Q. What causes Patellar Clunk Syndrome?
A. Patellar Clunk Syndrome is caused by the formation of fibrous tissue or scar tissue around the patella, which can catch on the femoral component of the knee implant, creating a clunking sensation.
Q. How is Patellar Clunk Syndrome treated?
A. Treatment options include physical therapy, corticosteroid injections, and in severe cases, arthroscopic surgery to remove the fibrous tissue or a revision surgery to adjust or replace the prosthetic components.
Q. Is Patellar Clunk Syndrome common after knee replacement?
A. No, Patellar Clunk Syndrome is relatively rare and typically occurs with older prosthetic designs, particularly posterior stabilized implants.
Summary and Takeaway
Patellar Clunk Syndrome, though uncommon, can be a frustrating complication after knee replacement surgery. Early diagnosis and treatment are crucial in managing this condition, and many patients experience relief with conservative measures or minimally invasive surgery. For patients with persistent symptoms, revision surgery may offer a permanent solution.
Clinical Insight & Recent Findings
A recent study systematically reviewed patellar resurfacing versus non-resurfacing in primary total knee arthroplasty (TKA), evaluating mid- and long-term outcomes.
The study found no significant difference in clinical function, pain, or anterior knee symptoms between the two groups at 2 years post-surgery. Both procedures resulted in substantial improvements in Knee Society Scores (KSS) and Visual Analog Scale (VAS) scores, with no significant increase in complications.
Despite trends favoring patellar resurfacing for reducing knee pain, this study suggests that it does not offer distinct advantages in terms of mid- and long-term effectiveness when compared to non-resurfacing techniques. (“Study of patellar resurfacing in TKA – See PubMed.”)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons specializing in knee surgeries, including joint replacements and revisions, are responsible for diagnosing and treating Patellar Clunk Syndrome. Physical therapists also play an essential role in post-surgical rehabilitation.
When to See a Specialist?
If you experience clunking, pain, or instability in the knee after a knee replacement, it is important to consult with your orthopedic surgeon to determine the cause and receive appropriate treatment.
When to Go to the Emergency Room?
Seek emergency care if you experience severe pain, swelling, or signs of infection after knee surgery, such as fever or increased redness and warmth around the joint.
What Recovery Really Looks Like?
Recovery involves a combination of physical therapy, pain management, and follow-up care. Most patients experience a significant reduction in symptoms and regain knee function within a few weeks to months.
What Happens If You Ignore It?
Ignoring Patellar Clunk Syndrome can lead to further damage to the knee joint, reduced functionality, and potentially require more extensive surgery down the line.
How to Prevent It?
While it may not be entirely preventable, adhering to post-surgical instructions, attending regular follow-ups, and engaging in physical therapy can help reduce the risk of developing Patellar Clunk Syndrome.
Do you have more questions?
How common is Patellar Clunk Syndrome after knee replacement surgery?
Patellar Clunk Syndrome occurs in a small percentage of patients undergoing knee replacement surgery, estimated to be around 1% to 3%.
Can Patellar Clunk Syndrome occur immediately after surgery, or does it develop over time?
It can happen either immediately after surgery or develop gradually over time as scar tissue forms around the joint.
Is Patellar Clunk Syndrome more common in certain types of knee replacement surgeries or implant designs?
Yes, certain factors like implant design, surgical technique, and patient-specific anatomy can influence the likelihood of developing Patellar Clunk Syndrome.
How long after knee replacement surgery does Patellar Clunk Syndrome typically develop?
It can vary from patient to patient, but symptoms typically arise within the first few months to a year after surgery.
Are there any specific risk factors that predispose someone to develop Patellar Clunk Syndrome?
Factors such as a history of knee trauma, previous surgeries, or underlying conditions like rheumatoid arthritis may increase the risk.
Can Patellar Clunk Syndrome lead to complications or further damage to the knee joint?
While it’s uncommon, severe cases of Patellar Clunk Syndrome can potentially lead to complications such as implant wear or instability if left untreated.
Is Patellar Clunk Syndrome more common in younger or older patients?
There’s no definitive age correlation, but younger patients with more active lifestyles may be at a slightly higher risk due to increased knee joint stress.
Are there any lifestyle modifications or activities that patients with Patellar Clunk Syndrome should avoid?
It’s generally advisable to avoid activities that exacerbate symptoms, such as high-impact sports or activities that involve repetitive knee bending.
Corticosteroid injections are generally safe but carry a small risk of complications such as infection, bleeding, or damage to surrounding tissues. Your doctor will discuss these risks with you before administering the injection.
Conservative treatments can be very effective, especially when combined with lifestyle modifications and medications. However, their success depends on the individual patient’s condition and response to treatment.
What are the potential risks or side effects associated with corticosteroid injections for Patellar Clunk Syndrome?
Corticosteroid injections are generally safe but carry a small risk of complications such as infection, bleeding, or damage to surrounding tissues. Your doctor will discuss these risks with you before administering the injection.
Are there any alternative treatments or complementary therapies that can help manage Patellar Clunk Syndrome?
Some patients find relief from complementary therapies such as acupuncture, chiropractic care, or herbal supplements. However, the effectiveness of these treatments can vary, and it’s essential to discuss them with your doctor before trying them.
How long does it take to recover from surgical interventions for Patellar Clunk Syndrome?
Recovery time varies depending on the type of surgery performed and the individual patient’s healing process. In general, patients can expect several weeks to months of rehabilitation and recovery.
Are there any long-term implications of Patellar Clunk Syndrome on knee function or mobility?
With proper treatment and management, most patients can regain full function and mobility in their knees. However, some individuals may experience persistent symptoms or limitations, especially if complications develop.
Can Patellar Clunk Syndrome recur after successful treatment?
While recurrence is uncommon, it’s possible for symptoms to return if the underlying cause is not adequately addressed or if new issues arise.
Are there any specific exercises or stretches that can help prevent Patellar Clunk Syndrome from recurring?
Yes, your physical therapist can recommend specific exercises to strengthen the muscles around your knee and improve joint stability, reducing the risk of recurrence.
How often should patients with a history of Patellar Clunk Syndrome follow up with their healthcare provider?
It’s essential for patients to attend regular follow-up appointments with their doctor to monitor their knee health and address any concerns promptly.
Are there any dietary or nutritional recommendations that can help manage Patellar Clunk Syndrome?
While there are no specific dietary guidelines for Patellar Clunk Syndrome, maintaining a healthy weight and eating a balanced diet can support overall joint health and recovery.
Can Patellar Clunk Syndrome affect other activities of daily living, such as walking or climbing stairs?
Yes, depending on the severity of symptoms, Patellar Clunk Syndrome can impact various activities of daily living. Physical therapy and lifestyle modifications can help minimize these effects.
Are there any assistive devices or braces that can help alleviate symptoms of Patellar Clunk Syndrome?
In some cases, a knee brace or orthotic device may provide additional support and stability, reducing the likelihood of the patella catching on the joint.
How soon after knee replacement surgery can patients resume normal activities like driving or returning to work?
The timeline for returning to normal activities varies depending on the individual patient’s recovery process and the type of surgery performed. Your doctor will provide specific guidelines based on your unique situation.
Are there any advancements in surgical techniques or implant designs that can reduce the risk of Patellar Clunk Syndrome?
Yes, ongoing research and advancements in orthopedic surgery continue to improve implant designs and surgical techniques, reducing the incidence of complications like Patellar Clunk Syndrome.
What should patients do if they experience a sudden increase in pain or swelling in their knee after surgery?
Sudden increases in pain or swelling should be promptly evaluated by a healthcare provider to rule out complications such as infection or implant failure.

