Microdiscectomy vs Nucleoplasty
Nucleoplasty and microdiscectomy are two minimally invasive surgical procedures aimed at relieving symptoms caused by lumbar disc herniation or bulging discs. Both procedures help to decompress the spinal nerve roots, which are often compressed by herniated disc material, leading to pain, numbness, and weakness in the legs. While both procedures are effective, they differ in their techniques, indications, and suitability for different types of disc problems.
How Common It Is and Who Gets It? (Epidemiology)
Lumbar disc herniation and disc bulging are common causes of lower back pain and sciatica, especially in individuals aged 30 to 50, and in those who perform heavy lifting or repetitive movements. Sciatica, characterized by pain radiating down the legs, is a frequent symptom of lumbar disc herniation. Approximately 10% of individuals with lumbar disc issues require surgical intervention, with the choice of procedure depending on the severity and type of the disc issue.
Why It Happens – Causes (Etiology and Pathophysiology)
A herniated or bulging intervertebral disc occurs when the soft, inner part of the disc (nucleus pulposus) pushes through cracks in the outer, tougher part (annulus fibrosus). This may lead to nerve compression, which causes symptoms such as radiating pain, numbness, and weakness in the lower limbs. The disc degeneration can result from:
-
Age-related wear and tear: The disc loses water content, leading to cracking and bulging.
-
Trauma or injury: Sudden pressure or repetitive stress on the spine can cause disc herniation.
-
Repetitive strain: Activities that put strain on the spine, such as lifting or poor posture, can also contribute to disc problems.
How the Body Part Normally Works? (Relevant Anatomy)
The lumbar spine is made up of five vertebrae (L1-L5) separated by intervertebral discs. The discs serve as shock absorbers and allow movement between vertebrae. The spinal cord runs through the spinal canal and nerve roots exit through openings called foramina. These nerves control sensation and movement in the legs, and when compressed by a herniated or bulging disc, they can lead to pain, numbness, and weakness in the affected area.
What You Might Feel – Symptoms (Clinical Presentation)
Common symptoms of lumbar disc herniation or bulging discs that may require nucleoplasty or microdiscectomy include:
-
Radiating Pain: Pain that travels from the lower back down through the buttocks and legs (sciatica).
-
Numbness and Tingling: Sensations of pins and needles in the legs or feet.
-
Weakness: Difficulty in moving the legs or feet, or clumsiness when walking.
-
Back Pain: Pain localized in the lower back, often worsened by movement or prolonged sitting.
How Doctors Find the Problem? (Diagnosis and Imaging)
To diagnose a herniated or bulging disc and determine the need for surgery, doctors typically use:
-
Physical Examination: To assess reflexes, strength, and nerve function.
-
MRI (Magnetic Resonance Imaging): The best imaging technique for visualizing soft tissues, including herniated discs and nerve compression.
-
CT Scan: Useful for detailed bone images, especially in the case of spinal stenosis.
-
X-rays: To check for structural abnormalities or degenerative changes.
-
Electromyography (EMG): Measures the electrical activity of muscles and helps to assess nerve function.
Classification
Nucleoplasty and microdiscectomy are both minimally invasive but vary in their applications:
-
Nucleoplasty: Primarily used for single-level disc bulges with less than 50% loss of disc height.
-
Microdiscectomy: Typically performed for larger herniations or extrusion of disc material. It involves removing herniated disc material that is pressing on the nerve root.
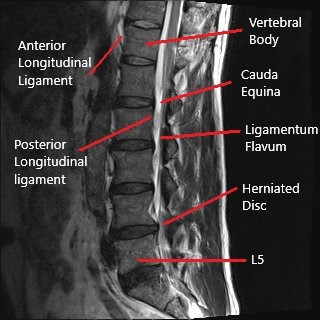
MRI of the lumbar spine in the sagittal section showing L4-L5 disc herniation.
Nucleoplasty vs Microdiscectomy
Nucleoplasty is a minimally invasive surgical technique that allows the surgeon to decompress the nerves. Minimally invasive surgery means there is minimum trauma to the structures surrounding the disc while performing the surgery. Nucleoplasty may be performed in an outpatient setting under local anesthesia. The patient remains semi conscious during the procedure while the area where the surgery is performed is anesthetized.
After adequate anesthesia, the surgeon inserts a needle in the involved intervertebral disc. The needle is guided by an external x-ray image intensifier. After the correct position of the needle is verified, the surgeon inserts a thermal-cautery/radiofrequency device. The thermal cautery or the radiofrequency device works by heating the nucleus pulposus.
The heating of the nucleus pulposus leads to shrinkage of the nucleus pulposus (nucleoplasty). The heat generation also leads to the remodeling of the annulus fibrous ring. The shrinkage of the pulposus along with the closure of the cracks leads to relief from disc bulge. After the needle is withdrawn, the entry site is closed with a bandage.
While the heat helps in the shrinkage of the nucleus pulposus, the surrounding tissues such as nerves, muscles, and bone is not damaged. The procedure involves minimum cutting of the tissues leading to a quicker rehabilitation. The patients are able to go home the same day of the procedure.
Microdiscectomy surgery involves a small incision and removal of the herniated disk under the direct vision of the surgeon. The procedure may be performed under general anesthesia in a hospital or in an outpatient setting under local anesthesia. The surgeon carefully separates the tissues to reach the involved spine segment. A small part of the lamina is removed to visualize the intervertebral disc.
The surgeon carefully retracts the spinal nerve roots and punches out small bits of the herniated intervertebral disk. The surgeon may also remove any bone spurs and widen the spinal canal in case of spinal stenosis. The procedure may be performed with an open traditional approach or using an endoscope (minimally invasive technique).
While nucleoplasty is less invasive than microdiscectomy, nucleoplasty can only be performed in limited circumstances. Nucleoplasty is only performed in patients in whom there is a single-level disc bulge. The procedure is limited to patients in whom the cause of symptoms is diagnosed to be solely because of the disk. Similarly, herniation and extrusion of the disc are managed with microdiscectomy rather than nucleoplasty. Nucleoplasty is only used to treat disc bulges with less than 50% loss of diameter.
Microdiscectomy may be combined with laminectomy surgery to relieve symptoms of spinal canal stenosis. Spinal lumbar fusion surgery is better suited in cases of spine instability. Both nucleoplasty and microdiscectomy are highly successful procedures for the management of discogenic pain. Speak with your spine surgeon to determine the procedure best suited for your condition.
Do you have more questions?
What is the main difference between microdiscectomy and nucleoplasty?
Microdiscectomy is a standard surgical procedure involving the removal of herniated disc material to relieve nerve pressure, often performed under general anesthesia. Nucleoplasty is a minimally invasive technique that uses thermal energy or radiofrequency to shrink and decompress the disc, suitable for smaller disc bulges.
Which procedure has a shorter recovery time?
Nucleoplasty generally has a shorter recovery time because it is minimally invasive, causing less tissue damage. Patients can often go home the same day and resume normal activities within a few days to weeks.
Can both procedures be performed under local anesthesia?
Yes, both procedures can be performed under local anesthesia. However, microdiscectomy is more commonly done under general anesthesia, especially in cases requiring more extensive surgery.
Is nucleoplasty suitable for all types of disc herniations?
No, nucleoplasty is best suited for patients with small, contained disc bulges without significant extrusion. It is not effective for large herniations or extrusions.
What are the risks associated with microdiscectomy?
Risks include infection, bleeding, nerve damage, spinal fluid leak, and recurrence of herniation. There is also a small risk of developing scar tissue that can compress the nerve.
Which procedure is more effective in relieving severe nerve compression symptoms?
Microdiscectomy is generally more effective for severe nerve compression symptoms due to its ability to remove larger disc herniations and address more complex issues.
How long does each procedure take?
Nucleoplasty typically takes about 30-60 minutes, while microdiscectomy can take 1-2 hours, depending on the complexity of the herniation and any additional procedures needed.
What kind of post-operative care is required for nucleoplasty?
Post-operative care for nucleoplasty includes rest, avoiding strenuous activities for a few days, and following a physical therapy regimen to strengthen the back and improve flexibility.
Can either procedure be performed on an outpatient basis?
Yes, both procedures can be performed on an outpatient basis, meaning the patient can go home the same day. However, microdiscectomy may require a short hospital stay in some cases.
What kind of post-operative care is required for microdiscectomy?
Post-operative care for microdiscectomy includes rest, wound care, gradually increasing activity, avoiding heavy lifting, and physical therapy to aid recovery and prevent future issues.
What are the chances of disc herniation recurrence after nucleoplasty?
The recurrence rate after nucleoplasty is relatively low, but it can vary depending on individual factors like lifestyle and adherence to post-operative care.
What are the chances of disc herniation recurrence after microdiscectomy?
Recurrence rates after microdiscectomy are around 5-15%. Following proper post-operative care and avoiding risk factors can reduce this risk.
Which procedure is better for older adults with degenerative disc disease?
Microdiscectomy may be more suitable for older adults with significant degenerative changes and larger herniations. Nucleoplasty is better for small, contained bulges.
Can nucleoplasty be performed on multiple disc levels?
Nucleoplasty is generally limited to single-level disc bulges. For multi-level issues, other procedures like microdiscectomy or fusion may be more appropriate.
How does each procedure affect the stability of the spine?
Nucleoplasty does not significantly affect spine stability as it is minimally invasive. Microdiscectomy can affect stability if a large portion of the disc or surrounding structures is removed, but it is often combined with techniques to preserve stability.
How soon can patients return to work after each procedure?
Patients can typically return to work within a few days to a week after nucleoplasty, depending on the nature of their job. After microdiscectomy, patients may return to work within 2-4 weeks, depending on recovery and job demands.
What is the success rate of nucleoplasty in relieving pain?
The success rate of nucleoplasty in relieving pain ranges from 70-80%, depending on patient selection and the specific condition being treated.
Can physical therapy help in recovery after these procedures?
Yes, physical therapy is crucial in the recovery process for both nucleoplasty and microdiscectomy. It helps improve strength, flexibility, and overall spinal health, reducing the risk of recurrence.
What is the success rate of microdiscectomy in relieving pain?
The success rate of microdiscectomy is generally high, with 85-95% of patients experiencing significant pain relief and improved function.

Dr. Mo Athar
