Cervical spine fusion- Minimally invasive
If cervical spine pain becomes severe enough to disrupt daily activities or is accompanied by swelling, tenderness, or redness, seeking medical attention is essential.
At Complete Orthopedics, our skilled cervical spine specialists excel in treating cervical spine pain using both surgical and non-surgical methods. We evaluate symptoms, identify the problem, and suggest suitable treatments, including surgery if necessary.
We cater to New York City and Long Island and work with six hospitals, offering state-of-the-art cervical spine surgery and comprehensive orthopedic services. Consultations with our orthopedic surgeons can be scheduled online or by phone.
Learn about common causes of cervical spine pain and the treatment options available, including when surgery is the best choice.
Overview
Anterior cervical decompression and fusion are performed to alleviate the symptoms of cervical radiculopathy, disc herniation, myelopathy, cervical fracture, degenerative arthritis, etc. Minimally invasive cervical decompression and fusion involve performing the surgery with special instruments, implants, and techniques to minimize damage to the structures around the cervical spine.
Anterior cervical decompression and fusion surgery involves accessing the cervical spine from the front of the neck. The surgeon removes the intervertebral disc and all the structures impinging upon the neural tissue causing the symptoms. The surgeon then introduces a cage between the vertebrae that is filled with bone graft material. The two or more vertebrae are then fixed with a plate and screws.
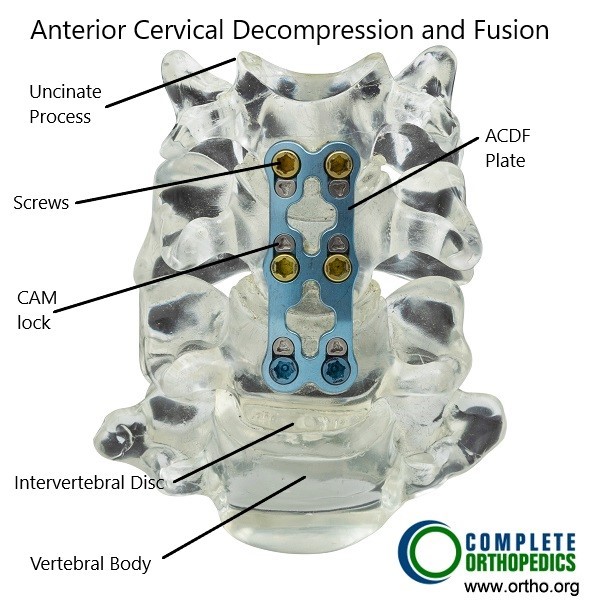
Anterior Cervical Decompression and Fusion
The majority of patients experience significant relief from the procedure and return to their normal activities in 6-8 weeks. The fusion of the vertebrae stabilizes the cervical spine segment and provides relief of symptoms.
The minimally invasive cervical decompression and fusion utilize a smaller incision to perform the decompression and fusion instead of the larger traditional approach. The smaller incision limits the amount of blood loss during the surgery. The complications associated with traditional surgery such as infection, nerve damage and difficulty swallowing occur less frequently with minimally invasive technique.
The minimally invasive surgery (MIS) technique also involves less cutting of the tissues to perform the fusion. The less cutting of tissue ensures a more rapid recovery compared to the traditional approach. The smaller incision also leads to smaller scar formation and therefore is more cosmetically appealing than the traditional approach.
The pain experienced after the surgery is less intense and lasts for less time compared to the traditional approach therefore minimizing the need for NSAIDs/narcotic medications. The minimally invasive cervical fusion may also be performed on an outdoor patient basis and most patients may return home the same day of the surgery. All the above benefits dramatically cut short the recovery period of cervical fusion surgery.
The procedure
During the procedure, a small incision of 1-2 inch is made on the front or side of the neck, the skin incision is usually made in the natural skin folds so the post surgery scar is minimally visible. The surgeon uses a special magnifying microscope to see through the small incision. Special instruments are used in minimally invasive techniques to gently retract the muscles and tissues to reach the cervical spine.
The surgeon then uses tiny instruments to remove the intervertebral disc and any other tissue (bone spurs, etc.) compressing the neural structures. The ends of the vertebrae are freshened to receive the bone cage (spacer) and the bone graft material. The spacer is used to maintain the space between the vertebrae and prevent compression of the neural tissue. Small plate and screws are then used to fix the vertebrae together.
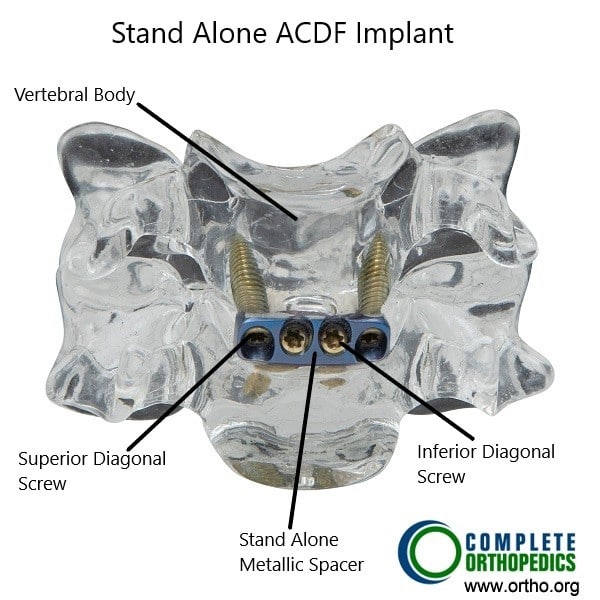
Stand Alone ACDF Implant.
Alternatively, a stand alone implant (spacer) may be used instead of the plate and screw construct. The stand alone implant spacer has screw holes that go diagonally towards the adjoining vertebrae. The stand alone implants offer the advantage of even smaller incisions in minimally invasive technique.
Benefits of Minimally Invasive Cervical Spine Fusion
The minimally invasive approach offers several significant benefits over traditional open surgery:
- Smaller Incisions: This reduces scarring and improves cosmetic outcomes.
- Less Tissue Damage: Minimally invasive techniques minimize damage to muscles and other soft tissues, which decreases postoperative pain and accelerates recovery.
- Reduced Blood Loss: The smaller surgical area means less bleeding during the procedure.
- Shorter Hospital Stays: Many minimally invasive surgeries are performed on an outpatient basis, and those requiring hospitalization typically involve shorter stays.
- Faster Recovery: Patients often experience quicker recovery times, allowing for a faster return to normal activities and work
Risks and Complications
Like any surgical procedure, minimally invasive cervical spine fusion carries potential risks:
- Infection: Despite precautions, there is always a risk of infection at the surgical site.
- Nerve Damage: There is a small risk of nerve injury, which could lead to pain, numbness, or, in rare cases, paralysis.
- Nonunion: Sometimes the bone graft does not fuse properly, which might require additional surgery.
- Implant Issues: Hardware used for stabilization can break or shift.
- Anesthesia Reactions: Some patients may have adverse reactions to anesthesia
Recovery and Aftercare
Postoperative care is crucial for a successful recovery. Patients are typically encouraged to walk and perform light activities shortly after surgery to promote healing and prevent complications. A neck brace may be prescribed to limit movement and support the spine as it heals. Physical therapy is often recommended to restore strength and flexibility.
Patients should follow their surgeon’s advice on activity restrictions, medications, and wound care to ensure proper healing. Regular follow-up appointments are necessary to monitor progress and address any concerns that may arise during recovery
Conclusion
Minimally invasive cervical spine fusion is a highly effective surgical option for treating certain cervical spine conditions. It offers numerous benefits, including reduced tissue damage, shorter recovery times, and smaller scars.
Do you have more questions?
How long does a minimally invasive cervical spine fusion surgery take?
The duration of the surgery can vary depending on the complexity of the case, but it typically takes between 1 to 3 hours.
What are the common indications for minimally invasive cervical spine fusion?
Common indications include herniated discs, degenerative disc disease, spinal stenosis, cervical spondylosis, and instability of the cervical spine.
How soon can I expect to see improvement in my symptoms after surgery?
Many patients experience significant relief from pain and other symptoms within a few days to weeks, but full recovery can take several months.
Are there any alternatives to minimally invasive cervical spine fusion?
Alternatives include conservative treatments like physical therapy, medications, and injections. Other surgical options include traditional open surgery or different minimally invasive procedures like disc replacement.
Can minimally invasive cervical spine fusion be performed on an outpatient basis?
Yes, depending on the patient’s overall health and the complexity of the surgery, it can be performed as an outpatient procedure, meaning no overnight hospital stay is required.
What kind of preoperative preparations are necessary?
Preoperative preparations may include stopping certain medications, quitting smoking, exercising, and undergoing imaging studies like X-rays or MRIs.
How long is the typical hospital stay after surgery?
If hospitalization is required, the stay is usually short, ranging from 1 to 2 days.
What are the signs of complications I should watch for after surgery?
Signs of complications include increased fluid leakage from the incision, fever, worsening pain, trouble breathing, and severe headache. Immediate medical attention should be sought if these occur.
Will I need physical therapy after the surgery?
Yes, physical therapy is often recommended to help restore strength, flexibility, and function during the recovery period.
How is a minimally invasive cervical spine fusion different from traditional open spine surgery?
Minimally invasive surgery uses smaller incisions, causes less muscle and tissue damage, leads to reduced blood loss, and typically results in shorter hospital stays and faster recovery times compared to traditional open surgery.
What materials are used for the bone graft in cervical spine fusion?
Bone graft materials can include autografts (patient’s own bone), allografts (donor bone), or synthetic materials.
How are the vertebrae stabilized during the fusion process?
The vertebrae are stabilized using implants such as screws, rods, and plates to hold them in place while the bone graft heals and fuses the bones together.
Is there a risk of adjacent segment disease (ASD) after fusion surgery?
Yes, there is a risk of ASD, where the segments adjacent to the fused area may experience increased stress and degeneration over time.
How soon can I return to work after the surgery?
Return to work depends on the nature of your job and your individual recovery. Many patients can return to light work within a few weeks, but more physically demanding jobs may require several months of recovery.
Are there any dietary restrictions after the surgery?
There are typically no specific dietary restrictions, but a balanced diet rich in nutrients can support the healing process.
What kind of pain management is used post-surgery?
Pain management may include medications such as analgesics, anti-inflammatory drugs, and muscle relaxants. Your surgeon will tailor a pain management plan to your needs.
Will I need a neck brace after the surgery?
A neck brace may be prescribed to support the cervical spine and limit movement during the initial healing phase.
What follow-up care is necessary after minimally invasive cervical spine fusion?
Follow-up care includes regular visits to your surgeon to monitor healing, manage any complications, and adjust your recovery plan as needed.
Can I travel by plane after the surgery?
Travel is generally safe after a brief recovery period, but it’s best to consult your surgeon for personalized advice based on your recovery progress.
Are there any lifestyle changes I need to make after the surgery?
Maintaining a healthy lifestyle, including regular exercise, good posture, and avoiding activities that strain the neck, can help prolong the benefits of the surgery.
What should I do if I experience new symptoms after surgery?
Any new or worsening symptoms should be reported to your surgeon immediately to rule out complications and ensure proper management.

Dr. Suhirad Khokhar
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.
