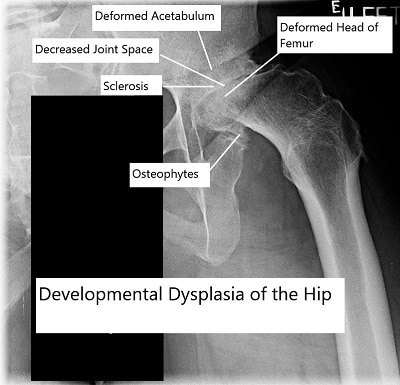
Developmental dysplasia of the hip is a condition that distorts normal hip bony anatomy during the formation of the hip joint in utero. It is due to abnormal fetal positioning and even with improved detection and screening techniques in infancy, developmental hip dysplasia is often very subtle and may be completely asymptomatic until it causes degenerative joint disease later on in life. Severe cases of hip dysplasia are usually detected during newborn screening or serial newborn examinations and so is far less common in the modern day, but in the developing world severe cases do still occur. The degeneration of the hip joint that occurs in dysplastic hips is unique, and in many cases leads to joint replacement surgery later on in life.
Developemental dysplasia of the hip
Causes
Numerous theories exist regarding the exact cause of abnormal joint anatomy in hip dysplasia, but the prevailing theory is that it is a result of the hip joint being positioned abnormally in utero and as such undergoing slightly abnormal anatomical development as compared to a normal hip joint.
Symptoms
The most common symptoms of hip dysplasia aren’t actually related to the dysplasia itself, but the arthritis that develops as a result of the abnormal anatomy. Pain, difficulty ambulating and decreased range of motion and stiffness are the hallmarks of arthritis pain – if these occur relatively early on in life such as the fourth or fifth decade of life, they are more likely to be related to dysplasia. Symptoms directly related to the dysplasia typically only occur in severe cases, and are usually quite obvious in infancy – as such they are much more easily identified and treated at that stage.
Treatment
Unfortunately due to the inherently abnormal underlying anatomy that hip dysplasia presents with, it is often the case that by the time the patient realizes they have hip dysplasia, they may be at the stage of that disease that requires surgical intervention as the best treatment option. With that being said, if hip dysplasia is found incidentally due to hip x-rays for other reasons then dysplasia may be managed conservatively and without surgery. If the patient has no symptoms then the dysplasia in and of itself does not require any treatment; however, if the dysplasia is causing pain and there are early signs of arthritic change then a same approach to these patients can be taken as would be the approach to managing patients with early arthritis for other reasons. Physiotherapy and anti-inflammatory medications will help control the symptoms, but ultimately these patients should be counseled that it is likely that in the future, they will require hip replacement surgery.
Duration
In early life, it is very important to pick up moderate-to-severe cases of hip dysplasia as, if these persist and/or are left untreated, they can result in highly abnormal anatomy that in some more severe cases can even preclude normal ambulation. Even in cases that are treated successfully the development of abnormal anatomy, although mitigated, is not eliminated entirely and such these patients may also be predisposed to develop arthritis at an earlier stage in their lives than the majority of osteoarthritis patients who do not have hip dysplastic features. The main consequence of leaving hip dysplasia untreated will be that the joint is predisposed to develop arthritic change at a much earlier age than one would wish for. This often leads to the need for surgery earlier on in life, which goes hand in hand with increasing the likelihood the patient will require revision surgery at some point later on in their life also.
Summary
Patients with a milder form of hip dysplasia will likely experience arthritis earlier in their lifetimes than is ideal , but are usually still good candidates for hip replacement surgery and ultimately will not require any different approach to any other hip replacement patient. Those with more severe forms of the disease should be treated on a case by case basis and counseled thoroughly by their healthcare practitioner as to what they can expect in terms of their likely outcomes from surgery. Ultimately, the goal of any surgery is to return the patient to a previous level of function that is desirable, achievable and acceptable.
Research Spotight
A recent study reviewed current approaches to treating hip dysplasia in adolescent patients, emphasizing that management decisions depend on both symptoms and radiographic findings. Nonoperative care—such as physical therapy, activity modification, and anti-inflammatory medications—is typically appropriate for mild or borderline cases (hips with limited undercoverage but no advanced arthritis).
When symptoms persist or imaging shows significant acetabular deficiency, periacetabular osteotomy (PAO) remains the gold-standard surgical treatment to restore hip stability and delay arthritis progression. The review also highlighted that combining PAO with hip arthroscopy can help address labral tears and cartilage problems in select patients, often improving long-term outcomes.
Overall, most adolescents treated appropriately—whether through therapy or surgery—achieve good function and reduced pain, reinforcing the importance of early detection and individualized management. (“Study on adolescent hip dysplasia management – see PubMed.”)
Some Input from Dr. Vaksha
Developmental dysplasia of the hip is a condition that distorts normal hip bony anatomy during the developmental stages of the hip when it is being formed in utero.
It is felt to be due to abnormal fetal positioning and even with improved detection and screening techniques early on in life, developmental hip dysplasia in many patients is often very subtle until it leads to degenerative joint disease later on in life.
More severe cases of this condition are usually detected during newborn screening or serial examinations of the newborn following their birth and so it is far less common now, but in the developing world you can still find severe cases of hip dysplasia. However, the most subtle cases may go easily missed and only manifest symptoms later on in life where they predispose the patient to degeneration of the hip joint and causes these patients to go on to require surgical intervention, which can include hip replacement surgery.
Hip Dysplasia prognosis, warning signs and causes
Hip dysplasia patients’ prognoses will differ based on the severity of the disease. There are patients with milder forms of the condition that may go their entire lives without ever realizing that they have dysplastic features in their hip. It would only be picked up if they ever had the hip x-rayed for alternative reasons.
However, some patients have sufficiently abnormal anatomy that the dysplasia predisposes them to develop arthritis in their hip in the later stages of life. This will generate the same symptoms as arthritis without dysplastic features of hip pain – difficulty ambulating and decreased range of motion and stiffness. Particular warning signs can include persistent and refractory hip pain early on in life (for example in the third or fourth decade) when degenerative changes begin to manifest within the joint as a result of the abnormal hip joint anatomy.
There are numerous theories with regards to the exact cause of the abnormal joint anatomy in hip dysplasia, but the prevailing theory is that it is a result of the hip joints being positioned abnormally in utero and as such undergoing slightly abnormal anatomical development as compared to a normal hip joint.
Hip Dysplasia Treatment Option
Unfortunately due to the inherently abnormal underlying anatomy that hip dysplasia presents with, it is often the case that by the time the patient realizes they have hip dysplasia, they may be at the stage of that disease that requires surgical intervention as the best treatment option.
With that being said, if hip dysplasia is found incidentally due to hip x-rays for other reasons then dysplasia may be managed conservatively and without surgery. If the patient has no symptoms then the dysplasia in and of itself does not require any treatment as such; however, if the dysplasia is causing pain and there are early signs of arthritic change then a same approach to these patients can be taken as would be the approach to managing patients with early arthritis for other reasons.
That is to stay that physiotherapy and anti-inflammatory medications will help control the symptoms, but ultimately these patients should be counseled that it is likely that in the future, they will require a surgical intervention of some type which can include hip replacement surgery.

Calcar proximal modular femoral component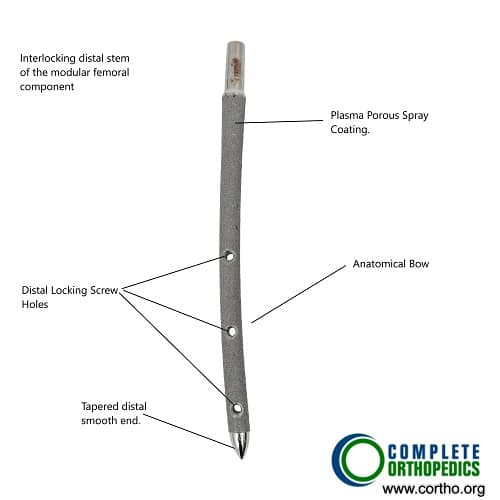
Modular distal stem of femoral component.
Modular components may be utilized during total hip replacement for the developmental hip dysplasia. The bone anatomy may be changed requiring special implants. Modular prosthetic implants allow adjustments during surgery for achieving greater stability.
What happens if Hip Dysplasia is left untreated?
In early life, it is very important to pick up moderate-to-severe cases of hip dysplasia as, if these persist and/or are left untreated, they can result in highly abnormal anatomy that in some more severe cases can even preclude normal walking and ambulation.
Even in cases that are treated successfully early on in life, the development of abnormal anatomy, although mitigated, is not eliminated entirely and such these patients may even be predisposed to develop arthritis at an early stage in their lives than the majority of osteoarthritis patients who do not have hip dysplastic features.
Ultimately, the main consequence of leaving hip dysplasia untreated will be that the joint is predisposed to develop arthritic change at a much earlier age than one would wish for. This often leads to the need for surgery earlier on in life, which goes hand in hand with increasing the likelihood the patient will require revision surgery at some point later on in their life also.
Who is a good candidate for Hip Dysplasia Surgery?
Essentially any patient who has developed symptoms as a result of arthritic change related to their underlying dysplasia would be considered to be a good candidate for surgery. Ideally, they should have failed conservative or nonoperative management of their arthritis first in the form of antiinflammatory medications and physiotherapy.
Provided that their medical history and physical examination leads their treating physician to suspect that their hip pain is as a result of arthritis related to the hip dysplasia, these patients would be considered good candidates for surgery. The severity of the dysplasia does not necessarily relate to suitability of the patient as a surgical candidate, indeed patients with mild dysplastic features may suffer the same level of symptoms as those with more severe dysplastic features and it is this that ultimately guides the decision to treat patients with surgery or not.
Hip Dysplasia Surgery Procedure
Hip replacement surgery for hip dysplasia patients is broadly similar to replacing anyone’s hip (with the potential for some added steps in more severe dysplasia cases). The vast majority of hip dysplasia patients who are in the milder end of the spectrum would essentially receive the same surgery as the patient who did not have any hip dysplasia anatomy and the procedure would not differ in any way.
Those with more severe deformities and more severely abnormal anatomy may require steps such as a subtrochanteric shortening osteotomy, and may even require specialist components that are specifically designed to deal with the inherent abnormal anatomy that hip dysplasia patients can often display. These include small components on the femoral side and larger or more complicated components on the acetabular side.
Hip Dysplasia Surgery Procedure Rate
Since the procedure is very much the same for non-dysplasia patients as it is for mild hip dysplasia patients, their success rates are broadly similar also. Patients with mild dysplastic features can expect to have the same success rates for this procedure as any other patients without dysplasia; that is to say greater than a 95% chance that surgery is successful and will have significantly improved symptoms and quality of life.
Those with more advanced versions of the disease do have a slightly lower success rate due to the fact that their anatomy is more significantly abnormal. That is not to say that the success rate is very low in this patient population, in fact it is still very high but the likelihood of a complication relating to the patient’s abnormal anatomy such as a hip dislocation or a fracture of the bone intraoperatively or postoperatively is greater and this should be explained to any patients with severe hip dysplasia considering undergoing hip replacement surgery. Despite this, patients with severe hip dysplasia have a success rate greater than 85% even with the considerations of the highly abnormal anatomy and the potential of postoperative complications.
Hip Dysplasia Surgery Risks
The risks of surgery are broadly similar to the risks for those patients undergoing hip replacements without hip dysplasia. The risk for postoperative complications such as infections and blood clots are identical and the presence of hip dysplasia does not affect these complication rates in particular. However, patients with more severe disease should be counseled with regards to their slightly increased complication rates in the form of postoperative dislocations and instability.
In particular, patients who are at the most severe end of the dysplasia spectrum may have issues relating to lengthening of that leg and they should be counseled that there is a slightly increased risk of nerve injury to the sciatic nerves as a result of lengthening their leg. This is particularly important for patients undergoing subtrochanteric shortening osteotomies and these patients should be judiciously monitored postoperatively for any neurological complications that may arise.
Hip Dysplasia Recovery and Timeframe
Recovering from hip replacement surgery in patients with hip dysplasia is almost identical to patients who received hip replacements who do not have hip dysplasia. Even patients with more severe anatomical abnormalities should expect to recover within the same kind of timeframe as those patients who had hip replacements for other reasons. Ultimately, the postoperative pain will persist for around 2 weeks, and should subside thereafter.
The patient will be able to mobilize and bear weight on the limb on the first postoperative day. The patients who require more invasive dissection of their musculature (which is typically the patients who have more severe forms of the disease) may require slightly longer to recover due to the fact that they have more muscle tissue disrupted as part of the surgery, but this should not grossly affect their recovery or make it significantly longer than the normal recovery time for hip replacement surgery.
By three months postoperatively, the pain should be almost completely subsided and the ambulation should be close to baseline of normal and by six months, the patient should essentially be fully recovered from the hip replacement surgery.
Hip Dysplasia Exercises
Your physical therapist will instruct you to broadly undergo the same sort of exercises that any hip replacement patient would be expected to perform. In particular, abductor strengthening exercises will be of great benefit and improve your gait and performance of the exercises during recovery.
In patients who have more severe anatomical abnormalities, it becomes increasingly important to adhere strictly to the postoperative hip precautions, which will include no adduction beyond neutral and no flexion beyond 90 degrees for up to 3 months. Avoiding excessive external rotation will also be an important restriction to adhere to, as all of these things will minimize the risk of the patient experiencing instability in the hip, which can be a challenging problem to address if it does occur.
Hip Dysplasia Surgery Host
As is a recurring theme with this topic, all hip dysplasia patients should likely not have to incur any greater costs related to their surgery than apply to other hip replacement patients. The increasing costs tend to occur when more specialist components and equipment are required and these are generally only reserved for patients who have more severe hip dysplasia that require specialist components for their anatomical abnormalities. Your surgeon can discuss these with you at greater length if they feel that special components are warranted.
Conclusion
Hip dysplasia in hip replacement patients can be summarized very simply in the following way; Patients with a milder form of disease will likely experience arthritis earlier in their lifetimes than is ideal , but are usually still good candidates for hip replacement surgery and ultimately will not require any different approach to any other hip replacement patient.
Those with more severe forms of the disease should be treated on a case by case basis and counseled thoroughly by their healthcare practitioner as to what they can expect in terms of recovery from the surgery, the components necessary and effect on cost this may have. Ultimately, the goal of any surgery is to return the patient to a previous level of function that is desirable, achievable and acceptable. In patients who suffer a loss of quality of life as a result of the changes in hip dysplasia, although different approaches may be required in more severe forms of the disease, they are all aimed at reproducing the same excellent results that hip replacement surgery yields.
Do you have more questions?
What questions should I ask my surgeon before undergoing hip replacement surgery for hip dysplasia?
Before undergoing hip replacement surgery for hip dysplasia, it’s important to ask your surgeon a variety of questions to ensure you have a thorough understanding of the procedure, expected outcomes, and postoperative care. Some questions to consider may include: What are the potential risks and benefits of hip replacement surgery in my case? What surgical approach and implant options are available, and which do you recommend for me? What is the expected timeline for recovery and return to normal activities? How many hip replacement surgeries for hip dysplasia have you performed, and what is your success rate? What postoperative precautions or restrictions will I need to follow, and for how long? How will pain management be addressed during and after surgery? Can you provide information about the hospital or surgical facility where the procedure will take place? Do you have any patient testimonials or outcomes data that I can review? These are just a few examples of questions you may want to ask your surgeon. Feel free to ask any additional questions or seek clarification on any concerns you may have about the surgery or recovery process.
Can physical activity or exercise worsen hip dysplasia symptoms, or is it beneficial?
Physical activity and exercise can play a beneficial role in managing hip dysplasia symptoms by improving muscle strength, joint stability, and overall function. However, certain high-impact or strenuous activities may exacerbate symptoms or increase the risk of joint injury, particularly in advanced cases of dysplasia. It’s essential to engage in activities that are appropriate for your individual condition and to consult with a healthcare provider or physical therapist before starting a new exercise regimen.
Are there any dietary changes or nutritional guidelines that can benefit hip dysplasia patients?
While there are no specific dietary changes or nutritional guidelines tailored specifically to hip dysplasia, maintaining a balanced diet rich in essential nutrients such as calcium, vitamin D, and protein can support overall bone health and joint function. If you have specific dietary concerns or medical conditions, it’s advisable to consult with a registered dietitian or healthcare provider for personalized recommendations.
How often should I follow up with my healthcare provider after hip replacement surgery?
Following hip replacement surgery, your healthcare provider will typically schedule regular follow-up appointments to monitor your recovery progress, assess joint function, and address any concerns or complications. The frequency of follow-up visits may vary depending on individual factors and surgical outcomes, but generally, appointments are scheduled at specific intervals during the first year post-surgery and may become less frequent as you progress.
Are there any long-term consequences or considerations I should be aware of after hip replacement surgery?
After hip replacement surgery, long-term considerations may include the need for periodic follow-up appointments, monitoring for implant wear or loosening, and ongoing maintenance of joint health through regular exercise, weight management, and adherence to postoperative precautions. While hip replacement surgery can provide significant and lasting relief from hip dysplasia symptoms, it’s essential to maintain a healthy lifestyle and follow your surgeon’s recommendations for long-term success.
How can I manage pain and discomfort associated with hip dysplasia while waiting for surgery?
Pain management strategies for hip dysplasia may include over-the-counter or prescription medications such as NSAIDs, acetaminophen, or muscle relaxants, as well as hot or cold therapy, gentle stretching exercises, and activity modification. Your healthcare provider can help develop a personalized pain management plan based on your specific needs and preferences.
Are there any alternative treatments or therapies I should consider before opting for surgery?
Before undergoing surgery, alternative treatments for hip dysplasia may include medications for pain management, physical therapy, assistive devices such as braces or orthotics, and lifestyle modifications. It’s essential to explore conservative options thoroughly before considering surgery, with guidance from a healthcare provider.
What are the expected outcomes or success rates of hip replacement surgery for hip dysplasia?
Overall, hip replacement surgery for hip dysplasia is associated with high success rates and significant improvements in pain relief, function, and quality of life. Success rates may vary depending on factors such as patient age, severity of dysplasia, surgical technique, and implant selection.
Are there any restrictions on activities or movements I should follow after hip replacement surgery?
Following hip replacement surgery, patients are usually advised to avoid high-impact activities, heavy lifting, and excessive bending or twisting of the hip joint. Specific activity restrictions may vary depending on surgical approach, implant type, and individual factors, and should be discussed with your surgeon.
How long does it typically take to recover from hip replacement surgery for hip dysplasia?
Recovery from hip replacement surgery varies from patient to patient but typically involves a period of restricted activity followed by gradual return to normal function. While some improvement may be noticed immediately after surgery, full recovery may take several months, with continued improvements over the following year.
Is there an optimal age or time to undergo hip replacement surgery for hip dysplasia?
The optimal timing for hip replacement surgery depends on various factors, including the severity of symptoms, functional limitations, overall health, and individual preferences. In general, surgery may be considered when conservative treatments fail to provide adequate relief and symptoms significantly impact daily life.
What are the potential risks or complications associated with hip replacement surgery for hip dysplasia?
Risks and complications of hip replacement surgery for hip dysplasia include infection, blood clots, dislocation, nerve injury, leg length inequality, implant loosening or wear, and rare but serious complications such as blood vessel injury or fracture. It’s essential to discuss these risks with your surgeon before undergoing surgery.
Can physical therapy help manage hip dysplasia symptoms, and what does a typical therapy regimen involve?
Yes, physical therapy can be an integral part of managing hip dysplasia symptoms. A physical therapist can design a tailored exercise program to strengthen hip muscles, improve flexibility, and optimize joint mechanics. Therapy may also include manual techniques, modalities such as heat or ice, and education on activity modification.
How does hip dysplasia impact daily activities and quality of life?
Hip dysplasia can significantly impact daily activities and quality of life, causing pain, stiffness, and limitations in mobility. Activities such as walking, climbing stairs, or getting in and out of chairs may become challenging, affecting overall function and well-being.
Are there any medications or supplements that can help slow the progression of hip dysplasia?
While medications and supplements cannot directly alter hip anatomy, certain treatments may help manage symptoms and improve overall joint health. These may include nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief, as well as calcium and vitamin D supplements to support bone health.
Is there a genetic component to hip dysplasia, and should I be concerned about passing it on to future generations?
There is evidence of a genetic component to hip dysplasia, with certain genetic factors contributing to an increased risk of developing the condition. If you have a family history of hip dysplasia or related conditions, it may be prudent to discuss genetic counseling with a healthcare provider when considering future family planning.
What imaging tests are used to diagnose hip dysplasia, and how accurate are they?
Imaging tests such as X-rays, CT scans, and MRIs are commonly used to diagnose hip dysplasia. X-rays are often the initial imaging modality and can provide detailed information about hip anatomy and alignment. CT scans and MRIs may offer additional insight, particularly in complex cases or to assess soft tissue structures.
Can hip dysplasia affect both hips, or is it typically isolated to one side?
Hip dysplasia can affect one or both hips, although it may be more common for dysplasia to occur asymmetrically, with one hip being more severely affected than the other. Bilateral hip dysplasia requires careful evaluation and management of both hips.
Are there specific risk factors that increase the likelihood of developing hip dysplasia?
Risk factors for hip dysplasia include family history, breech birth, firstborn status, female gender, and certain musculoskeletal conditions such as connective tissue disorders. Additionally, environmental factors such as swaddling techniques may contribute to hip dysplasia in infancy.
How likely is it for hip dysplasia to progress to the point of needing surgical intervention?
The likelihood of hip dysplasia progressing to the point of needing surgery varies depending on factors such as the severity of dysplasia, age, activity level, and response to conservative treatments. In some cases, surgery may be necessary to alleviate symptoms and improve hip function.
Are there any lifestyle modifications I can make to manage hip dysplasia symptoms without surgery?
Yes, certain lifestyle modifications can help manage hip dysplasia symptoms. These may include maintaining a healthy weight, avoiding high-impact activities, practicing hip-strengthening exercises recommended by a physical therapist, and using assistive devices like canes or walkers if needed.
Can hip dysplasia be detected later in life, even if it wasn't identified during childhood?
Yes, hip dysplasia can be detected later in life through imaging studies such as X-rays or MRIs, even if it wasn’t diagnosed in childhood. Symptoms like hip pain or discomfort may prompt further evaluation, leading to the discovery of hip dysplasia.
What are the early signs or symptoms that might indicate I have hip dysplasia?
Early signs of hip dysplasia may include hip pain, stiffness, or discomfort, especially during activities like walking, running, or prolonged sitting. You may also notice a reduced range of motion in the affected hip.

