Spinal Fusion vs. Microdiscectomy
Spinal fusion and microdiscectomy are two commonly used surgical treatments for lumbar spine conditions, particularly when conservative treatments fail. These procedures are designed to relieve pain caused by lumbar disc herniation or degeneration, with each addressing different aspects of spinal pathology. Spinal fusion is often used for cases involving instability or multiple disc herniations, while microdiscectomy is more suited for isolated herniations.
How Common It Is and Who Gets It? (Epidemiology)
Lumbar spine conditions such as disc herniation, degenerative disc disease, and spondylolisthesis are common, especially in adults between 30 and 60 years old. These conditions often lead to sciatica, characterized by radiating pain, numbness, or weakness in the legs. Around 10% to 15% of individuals with significant disc herniations require surgery, and the choice of procedure depends on factors like disc location, the degree of instability, and the severity of symptoms.
Why It Happens – Causes (Etiology and Pathophysiology)
-
Disc Herniation: When the inner part of the disc (nucleus pulposus) bulges out through a tear in the outer disc (annulus fibrosus), it can compress the spinal nerve roots, causing pain and other neurological symptoms.
-
Lumbar Stenosis: Narrowing of the spinal canal, often caused by age-related degenerative changes such as disc herniation, bone spurs, or thickened ligaments, leads to nerve compression.
-
Spondylolisthesis: A condition where one vertebra slips over another, often due to trauma or degenerative changes, leading to spinal instability.
-
Instability: Loss of disc height or damage to the spine following disc herniation can result in instability of the vertebral segment, often requiring spinal fusion for stabilization.
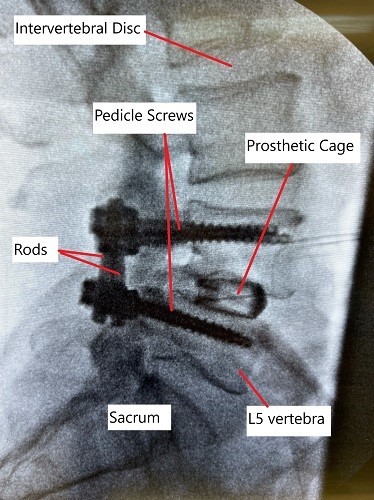
X-ray showing lumbar spine fusion at L4-L5 level.
How the Body Part Normally Works? (Relevant Anatomy)
The lumbar spine consists of five vertebrae (L1-L5) and intervertebral discs between them. The spinal cord runs through the spinal canal, and nerves exit through the foramina between the vertebrae. These nerves provide sensation and movement to the lower extremities. The intervertebral discs act as cushions between the vertebrae, absorbing shock and enabling movement. When a disc herniates, it may compress the nerve roots, leading to pain, numbness, and weakness in the legs.
What You Might Feel – Symptoms (Clinical Presentation)
-
Radicular Pain (Sciatica): Pain that radiates down the back of the legs, often caused by nerve compression.
-
Numbness or Tingling: Sensations in the legs or feet, typically on one side.
-
Weakness: Difficulty in moving the legs or performing tasks like standing or walking.
-
Back Pain: Persistent or intermittent pain localized in the lower back.
-
Loss of Reflexes: Decreased reflexes in the legs due to nerve involvement.
How Doctors Find the Problem? (Diagnosis and Imaging)
-
Physical Examination: Neurological tests to check for muscle weakness, reflexes, and sensory loss.
-
MRI (Magnetic Resonance Imaging): Provides detailed images of the discs, spinal cord, and nerve roots, identifying disc herniation and stenosis.
-
CT Scan: Offers clearer views of bony structures and can help assess spinal degeneration.
-
X-rays: Useful for detecting spinal misalignment, fractures, or degenerative changes.
-
Electromyography (EMG): Measures electrical activity in the muscles, helping to confirm nerve compression.
Classification
-
Microdiscectomy: Used primarily for single-level disc herniations where the nucleus pulposus is pressing on a nerve root.
-
Spinal Fusion: Often used for multiple disc herniations, spinal instability, spondylolisthesis, or lumbar stenosis, where the vertebrae are fused to prevent abnormal movement.
Other Problems That Can Feel Similar (Differential Diagnosis)
-
Spinal Stenosis: Narrowing of the spinal canal, leading to pressure on the spinal cord and nerve roots.
-
Facet Joint Syndrome: Degeneration or inflammation of the facet joints can mimic sciatica.
-
Piriformis Syndrome: Compression of the sciatic nerve by the piriformis muscle in the buttocks can cause sciatica-like symptoms.
-
Sacroiliac Joint Dysfunction: Inflammation of the sacroiliac joint can lead to lower back pain and leg symptoms.
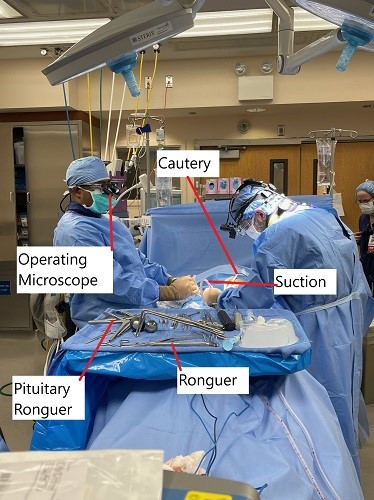
Intraoperative image showing microdiscectomy surgery.
Treatment Options
Non-Surgical Care
-
Physical Therapy: Strengthening and stretching exercises to improve spine mobility and reduce pressure on the nerves.
-
Medications: NSAIDs, muscle relaxants, or corticosteroids to manage pain and inflammation.
-
Epidural Steroid Injections: To reduce inflammation around the nerve roots and alleviate pain.
-
Nerve Blocks: For targeted pain relief in specific areas of the spine.
Surgical Care
-
Microdiscectomy: A minimally invasive procedure that removes the herniated part of the disc, relieving pressure on the nerve roots. Typically used for single-level disc herniations.
-
Spinal Fusion: A procedure that joins two or more vertebrae together using bone grafts and hardware (screws, rods) to stabilize the spine. This is often done in cases of spinal instability, spondylolisthesis, or multiple disc herniations.
Recovery and What to Expect After Treatment
-
Microdiscectomy:
-
Recovery time is generally shorter due to the minimally invasive nature of the procedure. Most patients return to light activities within 1-2 weeks and to normal activities in 4-6 weeks.
-
Full recovery may take several months, but many patients report significant pain relief and improved function.
-
-
Spinal Fusion:
-
Recovery from spinal fusion typically takes longer due to the more extensive nature of the procedure. Patients may require several weeks to months to recover fully, depending on the number of levels fused and whether there are complications.
-
Physical therapy is essential for rehabilitation, and weight-bearing restrictions may be imposed.
-
Possible Risks or Side Effects (Complications)
-
Microdiscectomy:
-
Recurrent Herniation: A small risk of the disc herniating again at the same level.
-
Nerve Injury: Though rare, there is a small risk of damaging the spinal nerves.
-
Infection: Though uncommon, there is a risk of infection at the incision site.
-
-
Spinal Fusion:
-
Non-fusion (Non-union): In some cases, the bones may fail to fuse properly, requiring additional surgery.
-
Hardware Complications: Broken or misaligned screws/rods may require revision surgery.
-
Adjacent Segment Degeneration: Increased stress on adjacent vertebrae can lead to further degeneration.
-
Long-Term Outlook (Prognosis)
-
Microdiscectomy: Most patients experience long-term relief from sciatica and can return to regular activities. However, there is a small risk of recurrent herniation, especially if the outer annulus of the disc is weakened during the procedure.
-
Spinal Fusion: Fusion surgery is highly effective for stabilizing the spine and preventing further disc herniation. However, the loss of motion in the fused segment can increase the risk of degeneration in adjacent segments over time.
Comparative Outcomes
Recurrent Lumbar Disc Herniation (RLDH) Treatment:
- Re-operative Rates: As noted, RD had higher re-operative rates due to recurrent herniation, while SF’s lower rates were primarily due to complications from adjacent segmental degeneration and implant issues.
- Clinical Improvement: Both procedures showed similar improvements in patient-reported outcomes, with no significant differences in ODI and JOA scores.
- Complications: Complications like dural tears were comparable between the two procedures, highlighting the necessity for surgical precision and postoperative care in both approaches.
Out-of-Pocket Costs
Medicare
CPT Code 63030 – Lumbar Microdiscectomy: $225.06
CPT Code 63020 – Cervical Microdiscectomy: $271.49
CPT Code 63040 – Thoracic Microdiscectomy: $335.83
CPT Code 22558 – Anterior Lumbar Interbody Fusion (ALIF): $368.50
CPT Code 22630 – Posterior Lumbar Interbody Fusion (PLIF/TLIF): $387.42
CPT Code 22612 – Posterior/Posterolateral Lumbar Fusion: $382.85
Under Medicare, 80% of the approved amount for these spinal procedures is covered once your annual deductible has been met. Patients are responsible for the remaining 20%. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield typically cover this 20%, meaning most patients have little to no out-of-pocket expense for Medicare-approved surgeries. These supplemental plans work closely with Medicare to close the payment gap for procedures such as microdiscectomy and lumbar fusion.
If you have secondary insurance—such as an Employer-Based Plan, TRICARE, or Veterans Health Administration—it acts as a secondary payer after Medicare. Once your deductible is satisfied, these plans often pay the remaining balance, including coinsurance. Most secondary plans have a small deductible of roughly $100 to $300, depending on the policy and whether your surgeon is in-network.
Workers’ Compensation
If your spinal condition is connected to a workplace injury, Workers’ Compensation will cover the full cost of evaluation, surgery, and recovery. You will have no out-of-pocket expenses for any approved treatment, including decompression, microdiscectomy, or fusion surgery.
No-Fault Insurance
If your back or neck injury is the result of an automobile accident, No-Fault Insurance will pay for all necessary medical and surgical treatment. The only possible out-of-pocket expense is a small deductible, depending on your policy. This includes coverage for discectomy and all types of lumbar fusion.
Example
Mark, a 62-year-old patient with a herniated lumbar disc, required a lumbar microdiscectomy (CPT 63030) and later a posterior lumbar fusion (CPT 22612). His Medicare out-of-pocket costs were $225.06 and $382.85. Because he carried supplemental Medigap coverage, the remaining 20% was paid in full, leaving him with no out-of-pocket expense for either surgery.
Frequently Asked Questions (FAQ)
Q. How long does it take to recover from microdiscectomy or spinal fusion?
A. Microdiscectomy has a quicker recovery, with many patients returning to light activities within 1-2 weeks. Spinal fusion recovery is longer, typically requiring 4-6 weeks for light activities and several months for full recovery.
Q. Which procedure is better for me: microdiscectomy or spinal fusion?
A. Microdiscectomy is typically preferred for isolated disc herniations, while spinal fusion is recommended for cases involving instability, multiple herniations, or conditions like spondylolisthesis. Your spine surgeon will assess your specific condition and recommend the best approach.
Q. What are the risks of these procedures?
A. Both procedures carry risks such as infection, nerve injury, and complications from surgery. Microdiscectomy tends to have a quicker recovery and fewer risks, but fusion may be necessary in cases of instability or recurrent herniation.
Summary and Takeaway
Both microdiscectomy and spinal fusion are highly effective surgeries for treating lumbar radiculopathy caused by disc herniation. Microdiscectomy is generally less invasive with a faster recovery time, making it suitable for patients with isolated disc herniations. Spinal fusion, while more invasive, is preferred for patients with instability, multiple herniations, or severe conditions like spondylolisthesis.
Who Performs This Treatment? (Specialists and Team Involved)
-
Spine Surgeons: Orthopedic or neurosurgeons specializing in spinal conditions.
-
Anesthesiologists: For anesthesia management during surgery.
-
Physical Therapists: To assist in post-operative rehabilitation and recovery.
When to See a Specialist?
If you experience persistent or worsening back pain, leg pain, numbness, or weakness, and conservative treatments have failed, consult a spine specialist to discuss surgical options.
When to Go to the Emergency Room?
Seek emergency care if you experience:
-
Sudden loss of bowel or bladder control.
-
Severe, unmanageable pain.
-
Sudden weakness or numbness in the legs or feet.
What Recovery Really Looks Like?
Microdiscectomy offers quicker recovery, while spinal fusion generally requires a longer recovery period. Both procedures significantly improve symptoms of sciatica, with full recovery taking several weeks to months.
What Happens If You Ignore It?
Ignoring symptoms of nerve compression can lead to worsening pain, permanent nerve damage, and loss of function. Early surgical intervention typically leads to better outcomes and faster recovery.
How to Prevent It?
Maintaining good posture, regular exercise, and proper lifting techniques can help prevent lumbar disc herniation.
Nutrition and Bone or Joint Health
A diet rich in calcium and vitamin D supports bone and disc health, helping to prevent degenerative changes in the spine.
Activity and Lifestyle Modifications
After surgery, low-impact activities like walking or swimming are encouraged to maintain flexibility and strength, while avoiding heavy lifting or high-impact exercises during recovery.
Do you have more questions?
What are the common complications associated with spinal fusion?
Common complications include increased blood loss during surgery, longer operative times, higher overall costs, risk of adjacent segmental degeneration, and potential for implant-related issues.
What are the primary benefits of spinal fusion for recurrent lumbar disc herniation?
The primary benefits of spinal fusion include providing long-term spinal stability, reducing the risk of future herniations at the operated level, and potentially lessening the need for future surgeries.
How do recovery times compare between spinal fusion and microdiscectomy?
Recovery times are generally shorter for microdiscectomy, with patients often resuming normal activities within a few weeks, whereas spinal fusion patients might need several months to fully recover.
Can spinal fusion and microdiscectomy be combined in a single procedure?
Yes, in some cases, a combined approach might be used where microdiscectomy is performed to remove the herniated disc material, followed by spinal fusion to stabilize the segment.
What factors influence the decision between spinal fusion and microdiscectomy?
Factors include the patient’s overall health, severity of spinal instability, previous surgical outcomes, presence of adjacent segmental degeneration, and the specific characteristics of the disc herniation.
What is the likelihood of requiring further surgery after a repeat discectomy?
The meta-analysis indicated a re-operative rate of 9.09% for repeat discectomy, mainly due to recurrent herniation.
What are the long-term outcomes of spinal fusion compared to microdiscectomy?
Long-term outcomes show that both procedures provide similar clinical improvements. However, spinal fusion offers better spinal stability, which might reduce the risk of future herniations at the operated level.
How does blood loss compare between spinal fusion and microdiscectomy?
Blood loss is significantly less in microdiscectomy (around 200-300 ml) compared to spinal fusion (over 500 ml), making microdiscectomy a less invasive option.
Is there a difference in pain relief between spinal fusion and microdiscectomy?
Both procedures provide significant pain relief, though spinal fusion might offer better results for back pain due to its stabilizing effect, while microdiscectomy is more effective for leg pain caused by nerve compression.
What is adjacent segmental degeneration, and why is it a concern with spinal fusion?
Adjacent segmental degeneration refers to the deterioration of spinal segments next to the fused vertebrae, which can occur because the fusion increases stress on these adjacent segments, potentially leading to further issues and surgeries.
What are the typical hospital stays for spinal fusion versus microdiscectomy?
Hospital stays for microdiscectomy average around 3 days, while spinal fusion patients might stay for over 6 days, reflecting the more extensive nature of the fusion surgery.
What are the primary causes for re-operation in spinal fusion?
Re-operations in spinal fusion are mainly due to adjacent segmental degeneration and implant removal issues.
How do operative times compare between the two procedures?
Operative times for microdiscectomy are shorter, averaging around 100 minutes, while spinal fusion procedures often take more than 150 minutes due to the complexity of the surgery.
Can spinal fusion lead to limitations in spinal movement?
Yes, spinal fusion limits movement at the fused segment, which can result in reduced flexibility and potential changes in biomechanics that might affect adjacent segments.
What is the significance of the Oswestry Disability Index (ODI) and Japanese Orthopaedic Association (JOA) scores in these studies?
These scores measure the degree of disability and pain relief. The studies found no significant differences in the improvement of these scores between the two procedures, indicating that both are effective in improving patient outcomes.
What follow-up care is required after spinal fusion or microdiscectomy?
Follow-up care for both procedures includes regular monitoring through physical exams and imaging studies, physical therapy to restore function and strength, and possibly lifestyle modifications to prevent recurrence.
How does patient satisfaction compare between spinal fusion and microdiscectomy?
Patient satisfaction is generally high for both procedures, with no significant differences reported in the studies. Satisfaction often depends on the resolution of symptoms and the absence of complications.
Are there any non-surgical alternatives to treat recurrent lumbar disc herniation?
Non-surgical alternatives include physical therapy, pain management through medications or injections, and lifestyle changes to reduce strain on the spine. However, these might be less effective for severe cases.
What advancements are being made in the surgical treatment of recurrent lumbar disc herniation?
Advancements include minimally invasive surgical techniques, better imaging technologies for precise diagnosis and planning, and the development of improved spinal implants and biologics to enhance fusion and recovery.
How do personal health and lifestyle factors impact the choice between spinal fusion and microdiscectomy?
Factors such as the patient’s age, activity level, overall health, presence of comorbidities, and personal preferences play a significant role in deciding the most appropriate surgical intervention.
What are the costs associated with spinal fusion compared to microdiscectomy?
Spinal fusion generally involves higher costs due to the complexity of the procedure, longer operative times, more extended hospital stays, and the use of implants and other materials. Microdiscectomy is less expensive due to its minimally invasive nature and shorter recovery period.
What is the prognosis for patients undergoing either procedure for recurrent lumbar disc herniation?
The prognosis for patients undergoing either spinal fusion or microdiscectomy is generally good, with most patients experiencing significant relief from symptoms and improved quality of life. The choice of procedure should be tailored to the patient’s specific condition and needs, with close follow-up to monitor for potential complications or recurrence.

Dr. Mo Athar
A seasoned orthopedic surgeon and foot and ankle specialist, Dr. Mohammad Athar welcomes patients at the offices of Complete Orthopedics in Queens / Long Island. Fellowship trained in both hip and knee reconstruction, Dr. Athar has extensive expertise in both total hip replacements and total knee replacements for arthritis of the hip and knee, respectively. As an orthopedic surgeon, he also performs surgery to treat meniscal tears, cartilage injuries, and fractures. He is certified for robotics assisted hip and knee replacements, and well versed in cutting-edge cartilage replacement techniques.
In addition, Dr. Athar is a fellowship-trained foot and ankle specialist, which has allowed him to accrue a vast experience in foot and ankle surgery, including ankle replacement, new cartilage replacement techniques, and minimally invasive foot surgery. In this role, he performs surgery to treat ankle arthritis, foot deformity, bunions, diabetic foot complications, toe deformity, and fractures of the lower extremities. Dr. Athar is adept at non-surgical treatment of musculoskeletal conditions in the upper and lower extremities such as braces, medication, orthotics, or injections to treat the above-mentioned conditions.
