Unstable Knee – Causes and Management
Knee instability, often described as a feeling of the knee “giving away” or buckling, can significantly impact daily life. This condition is commonly associated with pain, swelling, and difficulty with activities that require knee stability. Whether caused by ligament tears, meniscus injuries, or other underlying issues, understanding the causes and management strategies for knee instability is crucial for recovery and maintaining a good quality of life.
How Common It Is and Who Gets It? (Epidemiology)
Knee instability affects people of all ages but is particularly prevalent in athletes and individuals who engage in high-impact or twisting sports, such as football, soccer, and skiing. It is also common in older adults with degenerative knee conditions. Injuries to the knee ligaments, especially the anterior cruciate ligament (ACL), are a leading cause of knee instability. This condition often leads to functional limitations, including difficulty with walking, climbing stairs, or participating in recreational activities.
Why It Happens – Causes (Etiology and Pathophysiology)
Knee instability often results from injuries to the ligaments, meniscus, or other stabilizing structures within the knee. The most common causes include:
-
ACL injuries: Typically caused by sudden twisting or pivoting movements.
-
PCL injuries: Occur from direct force to the front of the knee, often seen in motor vehicle accidents or sports.
-
Medial Collateral Ligament (MCL) injuries: Caused by a force to the outer side of the knee, often in contact sports.
-
Meniscus tears: These can occur with rotational movements of the knee, leading to instability.
These injuries result in the loss of stability and function in the knee joint, contributing to a feeling of buckling.
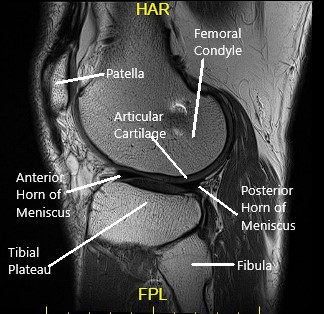
How the Body Part Normally Works? (Relevant Anatomy)
The knee joint is a hinge joint composed of the thigh bone (femur), shin bone (tibia), fibula, and kneecap (patella). The ligaments, cartilage, and menisci work together to provide stability and allow smooth movement.
-
Articular cartilage cushions and protects the bones.
-
Menisci serve as shock absorbers between the femur and tibia.
-
Ligaments, including the ACL, PCL, MCL, and LCL, stabilize the knee by preventing excessive movement.
-
Synovium produces synovial fluid, which lubricates the joint to ensure smooth motion.
When these structures are damaged, knee stability is compromised, leading to instability and an increased risk of injury.
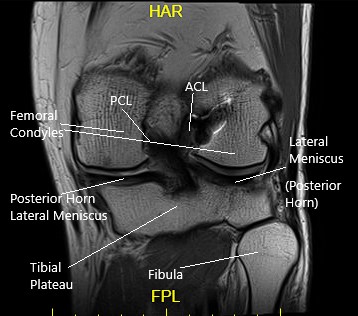
Ligaments
The ligaments of the knee along with the meniscus provide stability to the knee. Tears or rupture of the ligaments and menisci are the most common cause of knee buckling.
Anterior Cruciate Ligament (ACL)
The ACL runs from the front and middle of the tibia to the outer and backward side of the femur. The ligament provides stability mainly in the front and back of the knee. The ligament also stabilizes the rotatory movement of the knee.
Posterior Cruciate Ligament (PCL)
The PCL is present behind the knee joint. Along with ACL, it provides stability in the front and back of the knee. Similar to ACL, the PCL also provides rotational stability.
Medial & Lateral Collateral Ligaments
The medial collateral ligament provides stability on the inner side of the knee. Similarly, the lateral collateral ligament provides stability on the outer side of the knee.
Do you have more questions?
What exactly causes the knee to become unstable?
Knee instability is commonly caused by damage to ligaments such as the ACL, degenerative changes from osteoarthritis, or weakness in the muscles around the knee. It can also result from acute injuries or chronic wear and tear.
Are there specific exercises to prevent knee instability?
Yes, exercises focusing on strengthening the quadriceps, hamstrings, and calf muscles can help stabilize the knee. Balance exercises and core strengthening are also beneficial.
How is knee instability diagnosed?
Diagnosis typically involves a physical examination, patient history, and imaging tests like MRI or X-rays to assess ligament damage and joint status.
Can knee instability lead to other knee problems?
Yes, it can lead to increased wear and tear in the knee joint, exacerbate conditions like osteoarthritis, and increase the risk of falls and other injuries.
What are the treatment options for severe knee instability?
Severe instability might require surgical interventions such as ligament reconstruction or knee replacement, depending on the underlying cause.
How effective are knee braces in managing instability?
Knee braces can be very effective in providing support and stability, especially during activities that put stress on the knee.
What is the role of physical therapy in treating knee instability?
Physical therapy is crucial for strengthening the muscles around the knee, improving flexibility, and teaching stabilizing techniques to protect the joint.
Can knee instability be completely cured?
While some causes of instability can be effectively treated, chronic conditions like osteoarthritis may require ongoing management.
Is knee instability common in athletes?
Yes, athletes, particularly those involved in high-impact sports or activities that involve rapid direction changes, are at higher risk of developing knee instability.
What lifestyle changes can help manage knee instability?
Maintaining a healthy weight, avoiding high-impact activities, and regular knee-strengthening exercises can help manage symptoms.
How long does it take to recover from a procedure to correct knee instability?
Recovery times can vary widely based on the specific procedure, ranging from a few weeks to several months.
Are there age-specific concerns regarding knee instability?
Older adults may experience more pronounced effects due to muscle weakness and degenerative changes, while younger individuals may suffer from instability primarily due to injuries.
Can knee instability affect balance and coordination?
Yes, instability can significantly impact balance and coordination, increasing the risk of falls and affecting the ability to perform daily activities.
What are the signs that knee instability is worsening?
Increased frequency of knee giving way, heightened pain, swelling, and reduced mobility are signs that instability may be worsening.
Are there non-surgical treatments that can be effective?
Besides physical therapy and braces, treatments like corticosteroid injections, NSAIDs, and lifestyle modifications can be effective non-surgical options.
What is ACL reconstruction?
ACL reconstruction is a surgical procedure used to replace a torn anterior cruciate ligament, a common cause of knee instability.
How does obesity affect knee instability?
Obesity increases stress on the knee joints, exacerbating instability and associated symptoms like pain and reduced function.
Can knee instability be a sign of more serious health issues?
While it often relates to local issues within the knee, severe or unexplained instability should be evaluated to rule out other health problems.
What are the risks of surgery for knee instability?
Risks include infection, nerve damage, blood clots, and the potential for continued instability or pain.
How do I know if my knee instability is due to osteoarthritis?
A diagnosis typically involves evaluating symptoms like joint stiffness, pain during activity, and reviewing imaging studies.
What advancements are being made in treating knee instability?
Advances include new surgical techniques, better diagnostic tools, and developments in regenerative medicine like stem cell therapy.
Is swimming good for knee instability?
Yes, swimming is an excellent low-impact exercise that can strengthen the muscles around the knee without putting excessive stress on the joint.
How often should I perform stability exercises for my knee?
Frequency can vary based on individual needs, but generally, stability exercises should be performed 2-3 times per week, gradually increasing intensity and complexity under professional guidance.
What dietary considerations can help with knee health and stability?
A diet rich in anti-inflammatory foods such as omega-3 fatty acids, antioxidants, and adequate hydration can support joint health and potentially reduce symptoms related to knee instability.

Dr. Mo Athar
A seasoned orthopedic surgeon and foot and ankle specialist, Dr. Mohammad Athar welcomes patients at the offices of Complete Orthopedics in Queens / Long Island. Fellowship trained in both hip and knee reconstruction, Dr. Athar has extensive expertise in both total hip replacements and total knee replacements for arthritis of the hip and knee, respectively. As an orthopedic surgeon, he also performs surgery to treat meniscal tears, cartilage injuries, and fractures. He is certified for robotics assisted hip and knee replacements, and well versed in cutting-edge cartilage replacement techniques.
In addition, Dr. Athar is a fellowship-trained foot and ankle specialist, which has allowed him to accrue a vast experience in foot and ankle surgery, including ankle replacement, new cartilage replacement techniques, and minimally invasive foot surgery. In this role, he performs surgery to treat ankle arthritis, foot deformity, bunions, diabetic foot complications, toe deformity, and fractures of the lower extremities. Dr. Athar is adept at non-surgical treatment of musculoskeletal conditions in the upper and lower extremities such as braces, medication, orthotics, or injections to treat the above-mentioned conditions.
