Spinal fractures occur when one or more vertebrae—the bones of the spine—break or collapse. These injuries can range from mild compression fractures to severe, unstable fractures that threaten the spinal cord. They may result from trauma, such as a car accident or a fall, or from weakened bones due to conditions like osteoporosis. Some fractures heal with rest and bracing, while others require surgical stabilization to protect the spinal cord and restore spine alignment.
How Common It Is and Who Gets It? (Epidemiology)
Spinal fractures affect thousands of people each year. High-impact injuries, such as car accidents, sports injuries, or falls from height, are the leading causes in younger adults. In older adults, most spinal fractures result from osteoporosis, a condition that weakens bones and makes them more prone to collapse even after minor trauma. The thoracic and lumbar regions (middle and lower back) are most commonly involved.
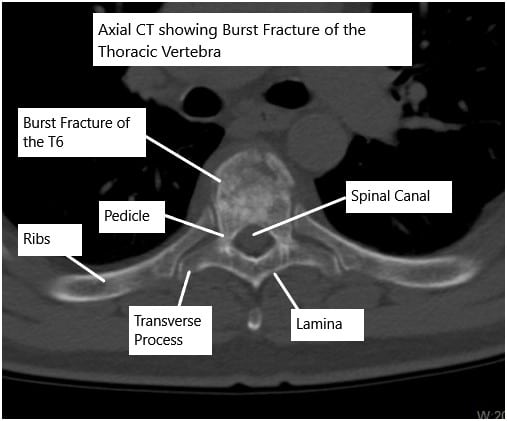
CT scan of the thoracic spine showing a burst fracture of the T6 vertebra.
The vertebral column consists of vertebra stacked on each other providing a safe conduit for the spinal cord. The spinal cord transmits signals from the brain that help in the movement of the four limbs. The spinal cord also gives branches known as spinal nerves at each level that travel to the part they supply.
Why It Happens – Causes (Etiology and Pathophysiology)
Spine fractures occur when the forces on the vertebrae exceed their strength.
Common causes include:
- Trauma: Motor vehicle accidents, falls, or sports injuries.
- Osteoporosis: Bone thinning that causes the vertebrae to collapse under normal pressure.
- Tumors or infections: Weaken bone structure, making it prone to fracture.
- Degenerative conditions: Chronic wear and tear that affects spinal stability.
In traumatic injuries, both bone and surrounding ligaments may be damaged, potentially compressing or injuring the spinal cord.
How the Body Part Normally Works? (Relevant Anatomy)
The spine consists of 24 movable vertebrae stacked to protect the spinal cord, which carries nerve signals between the brain and body. Each vertebra has a sturdy body in the front and an arch in the back that forms the spinal canal. Between the vertebrae lie intervertebral discs that cushion movement.
When a vertebra fractures, it can lose height or shift out of position. If the spinal cord or nerve roots are compressed, neurological symptoms such as weakness or numbness may appear.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms depend on the type and severity of the fracture:
- Sudden, severe back pain that worsens with movement
- Pain that radiates to the legs or arms
- Numbness or tingling in the limbs
- Muscle weakness or paralysis if nerves or the spinal cord are affected
- Loss of bladder or bowel control in severe cases
- Stooped posture or loss of height in osteoporotic fractures
Mild compression fractures may cause only localized pain, while major injuries can result in significant neurological deficits.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a physical exam and neurological assessment to check for weakness, sensation changes, or reflex loss. Imaging is crucial to identify the location and severity of injury:
- X-rays: Show bone alignment and vertebral collapse.
- CT scans: Provide detailed images of bone fragments and fracture patterns.
- MRI: Detects spinal cord compression, ligament injury, and soft-tissue damage.
In trauma cases, doctors will also check for other injuries to ensure comprehensive treatment.
Classification
Spinal fractures are classified by the mechanism and stability of the injury:
- Compression fractures: The front of the vertebral body collapses, common in osteoporosis.
- Burst fractures: The vertebra shatters into multiple pieces, sometimes pressing into the spinal canal.
- Flexion-distraction (Chance) fractures: Caused by sudden bending forward, often in car accidents.
- Fracture-dislocations: Severe injuries involving both fracture and misalignment of the vertebrae, often damaging the spinal cord.
Stable fractures may be managed without surgery, while unstable or displaced fractures typically require surgical fixation.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that can mimic spinal fractures include:
- Herniated discs
- Muscle or ligament strain
- Bone metastasis from cancer
- Severe arthritis or infection (osteomyelitis)
- Spinal deformities such as kyphosis from other causes
Imaging studies help differentiate these conditions from fractures.
Treatment Options
Non-Surgical Care
Stable fractures without spinal cord involvement are often treated conservatively:
- Bracing: A back or neck brace supports the spine while the bone heals.
- Pain management: Medications such as NSAIDs or acetaminophen.
- Physical therapy: Strengthening and posture exercises once pain improves.
- Rest: Limited activity until bone healing is confirmed.
Osteoporotic compression fractures may also be treated with minimally invasive procedures:
- Vertebroplasty: Injection of bone cement into the fractured vertebra.
- Kyphoplasty: Balloon inflation followed by cement injection to restore height.
Surgical Care
Surgery is required for unstable fractures or when there is spinal cord compression. Common procedures include:
- Laminectomy: Removing bone to decompress the spinal cord.
- Spinal fusion: Using screws, rods, and bone grafts to stabilize the fractured area.
- Instrumentation: Metal implants restore alignment and prevent further movement.
The surgical goal is to relieve pressure on the spinal cord and stabilize the spine for healing.
Recovery and What to Expect After Treatment
Recovery varies depending on injury severity:
- Conservative care: Most stable fractures heal within 8–12 weeks.
- Surgery: Hospital stays last several days, with gradual rehabilitation afterward.
- Rehabilitation: Physical therapy helps restore mobility, posture, and strength.
Some patients with severe injuries may need long-term therapy or assistive devices to regain independence.
Possible Risks or Side Effects (Complications)
Potential complications from spinal fractures or surgery include:
- Chronic pain or stiffness
- Deformity such as kyphosis (forward curvature)
- Nerve injury or paralysis
- Infection or bleeding
- Blood clots or non-union (failure of the bone to heal)
Careful follow-up, bracing, and rehabilitation minimize these risks.
Long-Term Outlook (Prognosis)
Most patients with mild to moderate fractures recover fully with appropriate treatment. However, severe fractures involving spinal cord damage may result in permanent weakness or paralysis. Early intervention, proper stabilization, and ongoing physical therapy greatly improve long-term outcomes.
Out-of-Pocket Costs
Medicare
CPT Code 22600 – Posterior Spinal Fusion (Cervical): $322.92
CPT Code 22612 – Posterior Spinal Fusion (Lumbar): $382.85
CPT Code 63001 – Decompression (Cervical Laminectomy): $307.25
CPT Code 63015 – Decompression (Thoracic Laminectomy): $370.64
CPT Code 63047 – Decompression (Lumbar Laminectomy): $271.76
CPT Code 22510 – Vertebroplasty (Thoracic): $401.05
CPT Code 22511 – Vertebroplasty (Lumbar): $400.74
CPT Code 22513 – Kyphoplasty (Thoracic): $1,249.27
CPT Code 22514 – Kyphoplasty (Lumbar): $1,243.52
Under Medicare, patients are responsible for 20% of the approved costs for these spinal procedures after meeting the annual deductible. Supplemental insurance plans such as Medigap, AARP, or Blue Cross Blue Shield typically cover this remaining 20%, which means patients often pay little to nothing out of pocket for Medicare-approved procedures. These supplemental plans are specifically designed to work with Medicare, offering comprehensive coverage for surgical interventions involving spinal fusion, decompression, and vertebral stabilization.
If you have secondary insurance—such as Employer-Based Plans, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer once Medicare has processed the claim. After your deductible is satisfied, the secondary plan may cover any remaining coinsurance or residual balance. Most secondary plans carry a small deductible, generally between $100 and $300, depending on your policy and provider network status.
Workers’ Compensation
If your spinal condition requiring fusion, decompression, or vertebroplasty/kyphoplasty resulted from a work-related injury, Workers’ Compensation will pay for all medical and surgical costs. This includes hospital care, instrumentation, and rehabilitation services. You will have no out-of-pocket expenses under a valid Workers’ Compensation claim.
No-Fault Insurance
If your spinal injury or fracture occurred as a result of an automobile accident, No-Fault Insurance will cover the full cost of all necessary spinal procedures, including laminectomy, fusion, vertebroplasty, or kyphoplasty. The only potential charge is a small deductible based on your individual policy terms.
Example
Susan, a 66-year-old patient with multiple spinal compression fractures, underwent thoracic kyphoplasty (CPT 22513) and lumbar fusion (CPT 22612). Her estimated Medicare out-of-pocket costs were $1,249.27 and $382.85, respectively. Since she had supplemental coverage through AARP Medigap, the remaining 20% coinsurance was paid in full, resulting in no out-of-pocket expenses for her treatment.
Frequently Asked Questions (FAQ)
Q. Are all spinal fractures serious?
A. Not all fractures are dangerous. Stable fractures without nerve injury often heal with rest and bracing.
Q. Can spinal fractures heal on their own?
A. Yes, mild compression fractures can heal naturally with proper support and rest.
Q. Will I be able to walk again after surgery?
A. Many patients regain full mobility after surgical stabilization, depending on the severity of spinal cord injury.
Q. Can osteoporosis-related fractures be prevented?
A. Yes. Managing bone health with calcium, vitamin D, exercise, and medications can reduce fracture risk.
Summary and Takeaway
Spinal fractures can result from trauma, osteoporosis, or disease. Symptoms include severe back pain, limited movement, and possible nerve problems. Diagnosis relies on imaging, and treatment ranges from bracing to surgery depending on stability. Most patients recover well with early management, rehabilitation, and bone health maintenance.
Clinical Insight & Recent Findings
A recent clinical review examined advances in the surgical stabilization of spinal fractures and spondylolisthesis, focusing on outcomes and instrumentation techniques. The study highlighted that thoracolumbar fractures—especially at the T11–L2 junction—are the most common, resulting from both high-impact trauma and osteoporosis.
Early surgical stabilization within 72 hours significantly reduced complications such as respiratory distress, sepsis, and prolonged hospitalization. For osteoporotic compression and burst fractures, minimally invasive procedures like vertebroplasty and kyphoplasty provided safe, effective pain relief and restored spinal alignment with low complication rates when performed carefully.
Innovations such as pedicle screw fixation, interbody cages, and robotic-assisted systems have improved surgical precision and recovery times. Despite these advancements, persistent postoperative pain and hardware complications remain challenges, emphasizing the need for tailored rehabilitation and careful long-term follow-up. (Study of spinal stabilization and fracture management – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is provided by orthopedic spine surgeons or neurosurgeons, often with support from rehabilitation specialists, physical therapists, and pain management physicians.
When to See a Specialist?
Consult a spine specialist if you experience:
- Severe back or neck pain after trauma
- Weakness, numbness, or loss of coordination
- Pain that doesn’t improve with rest
- Signs of spinal deformity or loss of height
When to Go to the Emergency Room?
Seek emergency care immediately if you have:
- Inability to move your legs or arms
- Loss of bladder or bowel control
- Severe, persistent back pain after an accident
What Recovery Really Looks Like?
Healing can take several months. Patients typically start with limited mobility, then gradually return to normal activities under supervision. Physical therapy helps rebuild strength and posture.
What Happens If You Ignore It?
Untreated spinal fractures can lead to deformity, chronic pain, or nerve damage. In severe cases, delayed care may result in permanent paralysis or loss of function.
How to Prevent It?
- Use seatbelts and proper protective gear during sports or driving.
- Prevent falls by keeping home spaces safe and well-lit.
- Treat osteoporosis with medication, exercise, and a calcium-rich diet.
- Avoid smoking and excess alcohol, which weaken bones.
Nutrition and Bone or Joint Health
Strong bones depend on calcium, vitamin D, and protein intake. Weight-bearing exercises and adequate hydration help maintain spinal strength and flexibility.
Activity and Lifestyle Modifications
After healing, continue low-impact exercises such as walking or swimming. Avoid heavy lifting and maintain good posture. For those with osteoporosis, regular follow-up bone scans ensure long-term spine health.
Do you have more questions?
What causes spine fractures?
Spine fractures can be caused by trauma such as car accidents, falls, sports injuries, or conditions like osteoporosis weakening the bones.
Can osteoporosis lead to spine fractures?
Yes, osteoporosis weakens bones, making them more prone to compression fractures, especially in older adults.
Are all spine fractures equally severe?
No, the severity of spine fractures varies depending on factors like the type of fracture, location, and involvement of the spinal cord or nerves.
How can I tell if I have a spine fracture?
Symptoms include severe back or neck pain, numbness or tingling, weakness, or loss of bladder or bowel control. Imaging tests like X-rays, CT scans, or MRI scans help diagnose spine fractures.
What are the treatment options for spine fractures?
Treatment varies from conservative management with pain relief and physical therapy to surgical intervention for severe fractures, depending on the type and severity.
What is involved in surgical treatment for spine fractures?
Surgical options include spinal fusion to stabilize the spine or decompression surgery to relieve pressure on the spinal cord or nerves.
How effective is rehabilitation after spine fracture treatment?
Rehabilitation, including physical therapy, is crucial for recovery, helping restore strength, flexibility, and function.
Can spine fractures lead to long-term complications?
Yes, complications can include chronic pain, deformity, neurological deficits, or even paralysis in severe cases involving spinal cord injury.
Can spine fractures be prevented?
Prevention strategies include managing osteoporosis with medication, lifestyle changes like proper nutrition and exercise, and fall prevention measures.
What are the risks associated with osteoporosis-related fractures?
Osteoporosis-related fractures can lead to chronic pain, deformity, loss of independence, and increased mortality, particularly in older adults.
Is surgery always necessary for spine fractures?
No, surgery is reserved for severe fractures with spinal instability or neurological involvement. Minor fractures may be managed conservatively.
How long does it take to recover from a spine fracture?
Recovery time varies depending on the severity of the fracture and the chosen treatment approach, but it typically involves weeks to months of rehabilitation.
Can spine fractures cause permanent disability?
Yes, severe spine fractures, especially those involving spinal cord injury, can result in permanent neurological deficits or paralysis.
Are there any complications associated with surgical treatment for spine fractures?
Complications can include infection, blood clots, nerve injury, or failure of the surgical hardware.
Can spine fractures recur after treatment?
While rare, spine fractures can recur, especially in individuals with osteoporosis or those involved in high-risk activities.
Is there a difference in treatment for different types of spine fractures?
Yes, treatment varies based on the type and severity of the fracture, as well as the patient’s overall health and individual circumstances.
Will I need to wear a brace after spine fracture treatment?
It depends on the type and severity of the fracture. Some patients may benefit from wearing a brace to support the spine during healing.
What is the success rate of surgical treatment for spine fractures?
Success rates vary depending on factors like the type of fracture, patient’s overall health, and surgical technique, but outcomes are generally favorable for appropriately selected patients.
Can spine fractures cause psychological effects?
Yes, coping with the physical limitations and potential long-term consequences of spine fractures can lead to psychological distress, including anxiety and depression
How can I prevent falls and reduce my risk of spine fractures?
Fall prevention measures include removing hazards at home, installing grab bars and handrails, wearing proper footwear, and participating in balance exercises.
Can spine fractures affect my ability to work or perform daily activities?
Yes, spine fractures, especially if they result in chronic pain or disability, can impact a person’s ability to work or engage in activities of daily living.
Will I need to take medication for osteoporosis indefinitely?
The duration of osteoporosis medication depends on individual risk factors, response to treatment, and ongoing assessment by a healthcare provider.
Are there any dietary supplements that can help with spine fracture recovery?
Calcium and vitamin D supplements are often recommended to support bone health and aid in fracture healing, but it’s essential to consult with a healthcare provider for personalized recommendations.
Can spine fractures lead to other spinal conditions like arthritis?
Yes, spine fractures can increase the risk of developing conditions like spinal arthritis, especially if the fracture causes joint instability or abnormal alignment.
What should I do if I suspect I have a spine fracture?
Seek immediate medical attention if you experience symptoms like severe back or neck pain, numbness or weakness, or loss of bladder or bowel control. A healthcare provider can perform a thorough evaluation and recommend appropriate treatment.

