Surgical Treatment of Sciatica of Lumbar Radiculopathy
Sciatica, or lumbar radiculopathy, is a condition characterized by pain radiating from the lower back into the legs, often accompanied by tingling, numbness, or weakness. The pain typically follows the distribution of the affected nerve root, commonly along the outer thigh, leg, and foot. This pain may occur unilaterally or bilaterally, depending on which nerve root is involved.
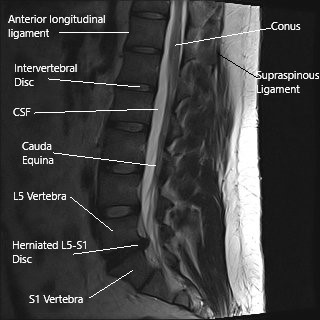
MRI of the lumbar spine in sagittal section showing herniated L5-S1 intervertebral disc.
How Common It Is and Who Gets It? (Epidemiology)
Sciatica is a common condition, with a lifetime prevalence of approximately 40%. It most often affects individuals between the ages of 30 and 50. Risk factors include aging, degenerative spinal conditions, obesity, and a sedentary lifestyle. Sciatica is more prevalent in men than women and is frequently associated with occupations that involve heavy lifting or prolonged sitting.
Why It Happens – Causes (Etiology and Pathophysiology)
The most common cause of sciatica is a herniated lumbar disc, where the disc material presses on the nerve root. Other causes include degenerative changes such as facet arthritis, spinal stenosis, or osteophyte formation. Sciatica can also result from synovial cysts or trauma. These conditions irritate or compress the nerve roots, leading to inflammation, ischemia, and pain.
How the Body Part Normally Works? (Relevant Anatomy)
The spine consists of vertebrae separated by intervertebral discs, which cushion and stabilize the spine. The nerve roots exit the spinal cord through the intervertebral foramen. The lumbar spine, in particular, is prone to disc herniation due to its weight-bearing function. The sciatic nerve, originating from the lumbar and sacral spinal roots, runs through the pelvis and down the legs, providing motor and sensory function.
What You Might Feel – Symptoms (Clinical Presentation)
Patients with sciatica often experience pain radiating from the lower back to the leg, typically following a specific dermatome. This pain can range from mild to severe and may be accompanied by tingling, numbness, and, in some cases, weakness in the affected leg. Symptoms are exacerbated by prolonged sitting, bending, or lifting.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis is typically clinical, based on a patient’s history and physical examination. Imaging tests like MRI are crucial for identifying disc herniations, degenerative changes, and other structural abnormalities in the lumbar spine. MRI scans in sagittal and axial views provide detailed images of the disc space, nerve roots, and the surrounding structures, helping guide treatment decisions.
Classification
Sciatica can be classified based on the underlying cause of the symptoms. Herniated disc-related sciatica is the most common type, but other causes include degenerative disc disease, spinal stenosis, and spondylolisthesis. The severity of the symptoms can range from mild discomfort to severe, debilitating pain with associated neurological deficits.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that can mimic sciatica include piriformis syndrome, lumbar muscle strain, and peripheral neuropathy. Additionally, other causes of lower back pain, such as sacroiliac joint dysfunction, can present with symptoms similar to sciatica.
Treatment Options
Non-Surgical Care
Non-surgical management includes medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and anticonvulsants like gabapentin. Physical therapy, acupuncture, and chiropractic care can also help alleviate symptoms. Steroid injections, such as epidural steroid injections or selective nerve root blocks, are sometimes used for more severe cases.
Surgical Care
Surgery is considered when conservative treatments fail or if there is significant neurological impairment. Surgical options include discectomy (removal of the herniated disc), microdiscectomy (minimally invasive surgery), and endoscopic discectomy. For patients with additional spinal instability, fusion surgery may be required.
MICRODISCECTOMY/ENDOSCOPIC DISCECTOMY
Discectomy can be either open or with the use of a microscope, also known as microdiscectomy. When discectomy is done with the use of endoscopy, then it is called endoscopic discectomy.
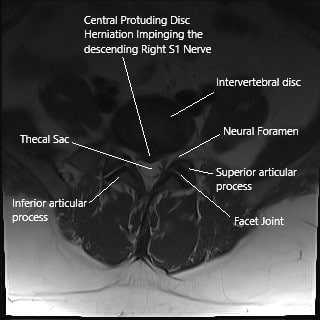
Axial section of the spine on MRI showing herniated intervertebral disc.
With the development of state of art instrumentation and better optics allowing visualization of magnification with the use of lens, microscope and endoscope, we are able to perform the surgery through smaller incisions allowing full recovery with minimal loss of blood, small incision and minimal morbidity.
In patients with isolated lumbar disc herniation without instability, microdiscectomy is the gold standard procedure in patients. This will also include decompressing the foramen and removing a part of lamina (foraminotomy and laminotomy).
Patients who have compression in the centers and bilateral disc herniations may need either procedure on both sides or removal of complete lamina (laminectomy) to allow for decompression.
For microdiscectomy, procedure is performed usually through a small incision less than 5 cm. A microscope is used for magnification and improved visualization with good illumination. The bone from the back of the spine, that is the lamina is removed to achieve a window to work (laminotomy) through which the disc can be reached and removed. The foramina was also cleared (foraminotomy).
In patients who have instability of the spinal segment, fusion surgery is performed. The bones are roughened (decorticated) and screws and rods are inserted so as to allow stability and healing and fusion to happen. Sometimes biologics like autogenous bone graft, allogeneic bone graft, substitutes like calcium triphosphate or stimulants like bone morphogenic protein or BMP can be used to enhance the fusion.
Patients who undergo microdiscectomy, foraminotomy, laminotomy, laminectomy can usually go home the same day or within 24 hours. These patients usually heal and recover faster and can be back to usual activity within 3 to 6 weeks. Patients who undergo fusion surgery take a longer recovery period and are usually in the hospital for 2 to 4 days.
Do you have more questions?
How do I know if my sciatica is severe enough to require surgery?
Surgery is generally considered if you have severe, persistent pain that has not responded to at least 6 weeks of conservative treatments, such as physical therapy, medications, or injections, and if the pain significantly interferes with your daily activities.
How effective is surgery in treating sciatica?
Surgery is highly effective in providing relief from leg pain associated with sciatica, especially in the short to medium term. Many patients experience significant improvement in pain and function within weeks of the procedure.
What are the risks associated with sciatica surgery?
Risks include infection, bleeding, spinal fluid leaks, nerve damage, and the possibility of requiring additional surgeries. However, these complications are relatively rare.
Will my sciatica symptoms return after surgery?
While surgery often provides long-lasting relief, some patients may experience a recurrence of symptoms, especially if there are ongoing degenerative changes in the spine.
What is the recovery time after sciatica surgery?
Recovery time varies depending on the type of surgery, but most patients can return to light activities within a few weeks. Full recovery, including a return to more strenuous activities, can take several months.
Can sciatica be treated without surgery?
Yes, many cases of sciatica can be successfully managed with non-surgical treatments, including physical therapy, medications, epidural steroid injections, and lifestyle modifications.
Is physical therapy required after surgery?
Yes, physical therapy is typically recommended after surgery to help strengthen the muscles, improve flexibility, and support a full recovery.
What are the chances that non-surgical treatments will fail?
Non-surgical treatments are effective for many people, but if there is significant nerve compression, these treatments might not provide sufficient relief, leading to the consideration of surgery.
How does sciatica surgery differ from other back surgeries?
Sciatica surgery, such as a discectomy or microdiscectomy, specifically targets the removal of the disc material or bone pressing on the sciatic nerve, unlike other back surgeries that may address broader spinal issues.
Will I need to stay in the hospital after sciatica surgery?
Most sciatica surgeries, especially minimally invasive ones, are done on an outpatient basis, allowing you to go home the same day. However, in some cases, an overnight stay may be required.
How can I manage sciatica pain before deciding on surgery?
Pain can often be managed with over-the-counter pain relievers, physical therapy, hot or cold packs, and avoiding activities that exacerbate the pain. In some cases, prescription medications or injections may be necessary.
What lifestyle changes can help prevent sciatica recurrence?
Maintaining a healthy weight, engaging in regular exercise to strengthen core muscles, practicing good posture, and avoiding activities that strain the lower back can help prevent sciatica recurrence.
Is sciatica surgery covered by insurance?
Most insurance plans cover sciatica surgery, especially if conservative treatments have been tried and failed. It’s important to check with your insurance provider for specific coverage details.
Can sciatica cause permanent nerve damage if left untreated?
Yes, in severe cases, prolonged nerve compression can lead to permanent nerve damage, resulting in chronic pain, numbness, or weakness in the affected leg.
What are the alternatives to surgery for managing sciatica?
Alternatives include physical therapy, chiropractic care, acupuncture, epidural steroid injections, and lifestyle modifications. These approaches can be effective, especially when combined.
What are the alternatives to surgery for managing sciatica?
Alternatives include physical therapy, chiropractic care, acupuncture, epidural steroid injections, and lifestyle modifications. These approaches can be effective, especially when combined.
How long does the pain relief last after sciatica surgery?
Many patients experience long-term relief from pain after surgery, though the duration can vary. Some patients may have relief for several years, while others might need additional treatment if symptoms recur.
Will I be able to return to work after sciatica surgery?
Most patients can return to work within a few weeks, depending on the type of work they do. Jobs that require heavy lifting or prolonged sitting might require a longer recovery period.
What should I expect during a sciatica surgery consultation?
During a consultation, the surgeon will review your medical history, conduct a physical examination, and possibly order imaging tests like an MRI to confirm the diagnosis and determine the best surgical approach.
Are there any dietary recommendations to help with recovery after surgery?
A balanced diet rich in nutrients that support healing, such as protein, vitamins, and minerals, is recommended. Staying hydrated and avoiding excessive weight gain are also important.
How can I differentiate between sciatica and other types of back pain?
Sciatica is characterized by pain that radiates from the lower back down the leg, often accompanied by numbness, tingling, or weakness. Other types of back pain might not follow this pattern and could be localized to the back or neck.
How is the success of sciatica surgery measured?
Success is typically measured by the reduction or elimination of leg pain, improvement in function and quality of life, and the ability to return to normal activities without significant limitations.
What are the signs that I might need a reoperation after sciatica surgery?
Signs that might indicate the need for reoperation include the return of severe pain, new or worsening symptoms, or the development of complications like infection or spinal fluid leaks
What should I do if I experience new symptoms after surgery?
If you experience new or worsening symptoms after surgery, such as increased pain, numbness, or signs of infection, contact your surgeon immediately for evaluation and possible intervention.
Can I travel shortly after sciatica surgery?
It’s advisable to wait at least a few weeks before traveling, especially if it involves long periods of sitting. Discuss your travel plans with your surgeon to ensure it’s safe based on your recovery progress.

Dr. Vedant Vaksha
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.
[et_pb_button admin_label="Button" button_url="https://www.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
