Lumbar radiculopathy, commonly known as sciatica, is often caused by a herniated disc in the lower back, leading to pain, numbness, tingling, and weakness in the legs. For patients who do not respond to conservative treatments such as physical therapy and medications, surgical intervention may be necessary. Tubular discectomy and microdiscectomy are two minimally invasive procedures used to treat this condition. Tubular discectomy, an advanced form of microdiscectomy, provides additional benefits such as less tissue disruption, quicker recovery, and reduced postoperative pain. Understanding the differences between these two techniques can help patients make an informed decision about their treatment.
Tubular discectomy vs Traditional microdiscectomy
The popular microdiscectomy surgery involves a small incision of 1.5 to 2 inches in the midline of the lower back directly on the involved disc. The surgeon uses an operating microscope to visualize the tissues through the small incision. The surgeon cuts the muscle attachments on the back of the vertebrae and carefully reaches the lamina and the ligamentum flavum.
The surgeon removes a small part of the lamina and uses instruments to remove the protruded part of the disc. The incision is closed in layers and the patients are able to go home the same day of the procedure.
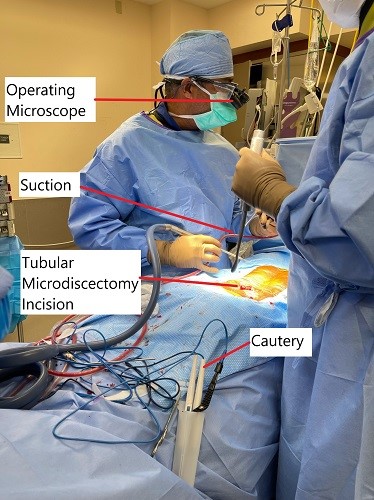
In a tubular discectomy, while the surgeon uses the same surgical technique, the muscles are separated instead of being cut. Serial dilators are used to separate the muscles. The surgeon gives a small incision about 1.8 to 2cm slightly away from the midline. A wire is passed under image intensifier control to the facet lamina junction.
Serial dilators are passed over the wire to separate the muscles and the tissues. The surgeon again uses a microscope to visualize the spine segment through the dilators. The herniated part of the intervertebral disc is removed and the incision is closed.
The patients are able to go home the same day of the procedure and are advised similar precautions as of microdiscectomy during the initial post-op period. Owing to the separation of muscles, patients undergoing tubular discectomy experience less postoperative back pain. The less cutting of the tissues leads to a faster rehabilitation as compared to microdiscectomy.
The patients may be able to return to their activities and work sooner as compared to traditional microdiscectomy. The intraoperative blood loss is less in the case of tubular discectomy and also the associated hospital stay. Patients report less use of narcotic pain medications after undergoing tubular microdiscectomy.
As with microdiscectomy, a tubular discectomy may be associated with complications such as a dural tear, damage to the spinal nerve roots, bleeding, infection, hematoma formation, and systemic complications such as blood clots or urinary tract infection.
Tubular discectomy presents a significant improvement over the traditional microdiscectomy but has a learning curve. The type of discectomy, open, micro, or tubular may be dependent upon the patient’s underlying anatomy and the disease process. A discussion with the operating surgeon may help you decide which procedure is best suited for you.
Tubular discectomy is a safe and successful procedure for the treatment of lumbar radiculopathy. The procedure offers several benefits in the form of less bleeding, less back pain, and early return to therapy and work as compared with traditional microdiscectomy.
The learning curve of tubular discectomy requires meticulous attention to position, manipulation of the nerves, and controlling bleeding. Fellowship-trained spine surgeons at Complete Orthopaedics may help you decide which procedure is best for you.
How Common It Is and Who Gets It? (Epidemiology)
Sciatica is a common condition affecting approximately 5-10% of adults, with the highest incidence occurring between the ages of 30 and 50. It is particularly prevalent in individuals who engage in activities that involve heavy lifting, poor posture, or repetitive motions. As a result, both microdiscectomy and tubular discectomy are frequently performed in patients with lumbar disc herniations that cause nerve compression, especially when conservative treatments fail.
Why It Happens – Causes (Etiology and Pathophysiology)
The primary cause of sciatica is a herniated intervertebral disc, where the soft inner part of the disc (nucleus pulposus) protrudes through the outer ring (annulus fibrosus), often compressing nearby spinal nerve roots. The degeneration of the disc with age, trauma, or repetitive stress weakens the outer layer, leading to disc bulging or herniation. When the disc compresses the spinal nerves, it results in pain, numbness, and weakness that radiates down the leg, known as lumbar radiculopathy.
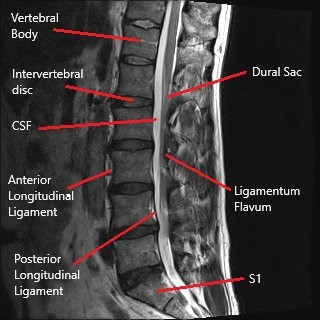
How the Body Part Normally Works? (Relevant Anatomy)
The lumbar spine consists of five vertebrae (L1-L5) separated by intervertebral discs. These discs act as cushions to absorb shock and allow movement. The spinal cord passes through the central canal, and nerve roots branch out from the spinal cord, exiting the spinal column through the intervertebral foramen. These nerves control sensation and movement in the lower body. A herniated disc can compress these nerve roots, leading to symptoms such as pain, tingling, and weakness.
What You Might Feel – Symptoms (Clinical Presentation)
Common symptoms of lumbar radiculopathy include:
- Sciatica: Radiating pain from the lower back down into one or both legs.
- Numbness or Tingling: Often described as “pins and needles” sensations in the buttocks, thighs, legs, or feet.
- Weakness: Difficulty moving the legs or feet, or instability when standing or walking.
- Back Pain: Pain localized to the lower back, often aggravated by sitting, standing, or bending.
How Doctors Find the Problem? (Diagnosis and Imaging)
- Physical Examination: A thorough exam is conducted to assess muscle strength, reflexes, and areas of pain or numbness.
- MRI (Magnetic Resonance Imaging): The most effective tool for visualizing soft tissues like discs and nerve roots. It can confirm disc herniation and nerve compression.
- CT Scan: Can provide detailed images of the bony structures in the spine.
- X-rays: Used to evaluate the alignment of the spine and detect any structural abnormalities.
- Electromyography (EMG): May be used to assess nerve function and confirm the presence of nerve damage.
Classification
- Microdiscectomy (MD): A minimally invasive procedure to remove herniated disc material that is pressing on the nerve root. It involves a small incision and is performed with the help of an operating microscope.
- Tubular Discectomy: A more advanced version of microdiscectomy, where serial dilators are used to gently separate muscles rather than cutting them. It requires a smaller incision and offers even less tissue disruption.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may mimic sciatica symptoms include:
- Spinal Stenosis: Narrowing of the spinal canal that compresses the spinal cord and nerves.
- Piriformis Syndrome: Compression of the sciatic nerve by the piriformis muscle in the buttocks.
- Sacroiliac Joint Dysfunction: Pain originating from the sacroiliac joint, often mistaken for sciatica.
- Facet Joint Syndrome: Degeneration of the facet joints, causing lower back pain and radiating symptoms similar to sciatica.
Treatment Options
Non-Surgical Care
- Physical Therapy: Strengthening exercises and stretching to alleviate pressure on the nerves and reduce pain.
- Medications: Pain relievers (NSAIDs), muscle relaxants, and corticosteroids to reduce inflammation.
- Epidural Steroid Injections: To provide targeted pain relief and reduce inflammation around the nerve roots.
Surgical Care
- Microdiscectomy (MD): The surgeon removes the herniated disc material through a small incision using a microscope. This procedure is ideal for cases of disc herniation that have not responded to conservative treatments.
- Tubular Discectomy: An advanced, minimally invasive procedure that uses serial dilators to gently separate muscles and access the herniated disc. The incision is smaller, and the technique results in less muscle damage and quicker recovery.
Recovery and What to Expect After Treatment
- Microdiscectomy:
- Recovery time is typically shorter, with most patients able to return to light activities within 1-2 weeks. Full recovery may take 4-6 weeks.
- The patient can usually go home the same day of the surgery.
- Tubular Discectomy:
- This procedure offers an even quicker recovery due to less muscle disruption. Most patients can return to light activities within a week and resume normal activities within 2-4 weeks.
- Similar to microdiscectomy, tubular discectomy is an outpatient procedure, and patients are typically discharged the same day.
Possible Risks or Side Effects (Complications)
- Microdiscectomy:
- Infection: Risk at the surgical site, though relatively low.
- Nerve Injury: Rare, but possible during the procedure.
- Recurrent Herniation: A small percentage of patients may experience another herniation at the same level.
- Dural Tear: Accidental tear of the dura (the membrane around the spinal cord), requiring repair.
- Tubular Discectomy:
- Infection: A low risk, given the minimally invasive approach.
- Nerve Injury: Rare, as the surgeon uses more precise techniques and instruments.
- Recurrent Herniation: Can occur if the disc is not adequately removed.
- Dural Tear: Though rare, the risk exists due to the nature of the procedure.
Long-Term Outlook (Prognosis)
Both microdiscectomy and tubular discectomy are highly successful in relieving sciatica caused by lumbar disc herniation. The majority of patients experience significant pain relief and return to normal activities. However, there is a small risk of re-herniation or degeneration of adjacent discs over time, especially if the patient does not follow post-operative care instructions.
Out-of-Pocket Cost
Medicare
CPT Code 63030 – Tubular Discectomy (Minimally Invasive Lumbar Discectomy): $225.06
Under Medicare, 80% of the approved amount for this procedure is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—usually cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved minimally invasive discectomy procedures. These supplemental plans work directly with Medicare to ensure full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it functions as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on the specific policy and network status.
Workers’ Compensation
If your lumbar spine condition requiring tubular discectomy surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your lumbar spine injury resulting in tubular discectomy is caused by a motor vehicle accident, No-Fault Insurance will cover the full cost of the procedure. The only possible out-of-pocket expense may be a small deductible depending on your individual policy terms.
Example
Susan, a 59-year-old patient with lumbar disc herniation, underwent minimally invasive tubular discectomy (CPT 63030) to relieve her sciatica and restore spinal function. Her estimated Medicare out-of-pocket cost was $225.06. Since Susan had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving her with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. What’s the difference between microdiscectomy and tubular discectomy?
A. The main difference is that tubular discectomy uses smaller incisions and causes less muscle disruption, leading to quicker recovery and less postoperative pain compared to microdiscectomy.
Q. How long does recovery take for tubular discectomy?
A. Recovery for tubular discectomy is typically quicker than microdiscectomy, with most patients returning to light activities within 1-2 weeks and full recovery within a few weeks.
Q. Are there risks associated with tubular discectomy?
A. While rare, risks include infection, nerve injury, and recurrent herniation. However, tubular discectomy is minimally invasive, which reduces the overall risk compared to open surgery.
Summary and Takeaway
Tubular discectomy is an advanced, minimally invasive technique for treating lumbar radiculopathy caused by herniated discs. It offers advantages over traditional microdiscectomy, such as reduced blood loss, quicker recovery, and less postoperative pain. However, it requires a high level of surgical precision, and patients should discuss with their surgeon whether this technique is suitable for their condition.
Clinical Insight & Recent Findings
A recent study examined the effectiveness of Microscopic Tubular Discectomy (MTD) for treating Far Lateral Lumbar Disc Herniation (FLLDH), focusing on improvements in pain and mobility.
The review found that MTD significantly reduced both leg and back pain, with post-surgery VAS scores showing marked improvement. Additionally, mobility, as assessed by the Oswestry Disability Index (ODI), also improved substantially. The surgery was associated with minimal blood loss, shorter operation times, and quicker recovery compared to traditional discectomy methods.
Despite its effectiveness, the study highlighted the need for larger, controlled studies to confirm the long-term benefits of MTD over other discectomy techniques. (“Study of the effectiveness of Microscopic Tubular Discectomy for FLLDH – See PubMed.”)
Who Performs This Treatment? (Specialists and Team Involved)
Both procedures are performed by:
- Spine Surgeons: Orthopedic or neurosurgeons specializing in spinal disorders.
- Anesthesiologists: For anesthesia management during surgery.
- Physical Therapists: To assist with post-operative rehabilitation and recovery.
When to See a Specialist?
If you experience persistent or worsening back pain, radiating leg pain, or weakness, and conservative treatments have failed, it may be time to consult a spine specialist to discuss surgical options.
When to Go to the Emergency Room?
Seek emergency care if you experience:
- Sudden loss of bladder or bowel control.
- Severe, unmanageable pain.
- Sudden weakness or numbness in the legs or feet.
What Recovery Really Looks Like?
Tubular discectomy offers the quickest recovery, with most patients resuming light activities within 1-2 weeks. Microdiscectomy recovery typically takes 2-4 weeks, with full recovery in several months.
What Happens If You Ignore It?
Ignoring symptoms of herniated discs can lead to worsening pain, permanent nerve damage, and loss of function. Early intervention through surgery can prevent these long-term issues.
How to Prevent It?
Maintaining a healthy weight, practicing good posture, and strengthening the muscles that support the spine can help prevent disc herniation and the need for surgery.
Nutrition and Bone or Joint Health
A balanced diet rich in calcium and vitamin D supports bone health and can help prevent degenerative changes in the spine.
Activity and Lifestyle Modifications
After surgery, engage in low-impact activities like walking or swimming to maintain flexibility and strength, while avoiding heavy lifting or high-impact exercises during recovery.
Do you have more questions?
What causes lumbar radiculopathy?
It is often caused by degenerative disc disease, where age-related wear and tear lead to disc herniation, or by trauma from falls, repetitive actions, or heavy lifting.
What are the symptoms of lumbar radiculopathy?
Symptoms include radiating leg pain, numbness, tingling sensations, and sometimes weakness in the lower extremities.
How is lumbar radiculopathy diagnosed?
Diagnosis is typically made through a combination of patient history, physical examination, and imaging studies such as MRI or CT scans.
What are the non-surgical treatments for lumbar radiculopathy?
Non-surgical treatments include pain medications, physical therapy, heat/cold therapy, and lifestyle modifications to reduce strain on the spine.
When is surgery recommended for lumbar radiculopathy?
Surgery is recommended when conservative treatments fail to relieve symptoms, and the patient’s quality of life is significantly affected by persistent pain and neurological deficits.
What is discectomy?
Discectomy is a surgical procedure to remove the herniated portion of an intervertebral disc that is compressing a nerve root.
What is the difference between microdiscectomy and tubular discectomy?
Microdiscectomy involves a small incision and uses an operating microscope, while tubular discectomy uses even smaller incisions and serial dilators to separate muscles rather than cutting them.
What are the benefits of microdiscectomy?
Benefits include smaller incisions, less muscle damage, reduced postoperative pain, and faster recovery compared to traditional open discectomy.
Are there any risks associated with tubular discectomy?
Yes, risks include dural tears, nerve root damage, bleeding, infection, and systemic complications like blood clots or urinary tract infections.
How do surgeons handle CNR during tubular discectomy?
Surgeons must be vigilant during preoperative imaging and intraoperative procedures, ensuring thorough decompression and careful manipulation of the nerves to avoid complications.
What is the typical recovery time after a tubular discectomy?
Patients typically experience a faster recovery, with many returning to normal activities and work within a few weeks, depending on the extent of the surgery and the individual’s health.
How effective is tubular discectomy in relieving symptoms of lumbar radiculopathy?
Tubular discectomy is highly effective in relieving symptoms, with most patients experiencing significant improvement in pain and neurological function.
Can lumbar radiculopathy recur after discectomy?
Yes, there is a risk of recurrence, especially if the underlying degenerative changes in the spine continue or if the patient resumes activities that strain the spine.
How do patients prepare for a tubular discectomy?
Preparation includes preoperative consultations, imaging studies, discontinuing certain medications, and following specific instructions regarding diet and activity before surgery.

