A synovial facet cyst is a small, fluid-filled sac that forms in the facet joint of the spine—most often in the lower back (lumbar region). These cysts develop due to degenerative changes in the spine and may compress nearby nerves, causing lower back pain and radiating leg pain (sciatica).
While some facet cysts cause no symptoms, others can lead to spinal canal narrowing (stenosis) and significant discomfort.
How Common It Is and Who Gets It? (Epidemiology)
Synovial facet cysts are uncommon but typically occur in older adults (over 50 years) due to arthritis and wear-and-tear changes in the spine. They are most frequently found at the L4–L5 level, where motion and degeneration are greatest. Both men and women are equally affected.
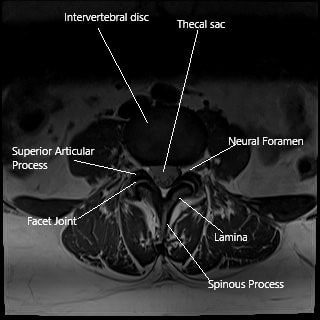
MRI axial section showing the facet joint.
Why It Happens – Causes (Etiology and Pathophysiology)
Facet joints connect the vertebrae at the back of the spine and allow for smooth movement. They are surrounded by a capsule that produces synovial fluid—a lubricant that helps the joints move easily.
With aging and degeneration:
- Intervertebral discs lose height, putting more stress on facet joints.
- Facet arthritis develops, leading to inflammation and joint instability.
- The capsule may produce excess synovial fluid, which can form a pocket or cyst.
This cyst may press on nearby nerve roots or the spinal canal, causing pain and neurological symptoms.
Occasionally, bleeding into the cyst (facet cyst hematoma) causes rapid symptom worsening.
How the Body Part Normally Works? (Relevant Anatomy)
The facet joints are located behind each vertebra and guide motion in the spine. Each joint has smooth cartilage and is enclosed by a capsule filled with synovial fluid for lubrication.
When degeneration occurs, the capsule may weaken, bulge, and form a cyst. This cyst can intrude into the spinal canal, reducing the space available for nerves.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms depend on the cyst’s size and location:
- Lower back pain—often worse with standing or walking.
- Leg pain (sciatica): Radiating pain from the lower back into one or both legs.
- Numbness or tingling in the legs or feet.
- Weakness in the legs if the cyst compresses nerve roots.
- Neurogenic claudication: Pain in the buttocks and legs that worsens with walking and improves when sitting or bending forward.
- Sudden worsening of pain if bleeding occurs inside the cyst.
Symptoms are often similar to spinal stenosis or a herniated disc.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a physical exam and neurological assessment.
- MRI: The gold standard imaging test for detecting facet cysts and evaluating nerve compression.
- CT scan: May be used for detailed bone structure evaluation or to guide injections.
- X-rays: Can show degenerative changes or joint instability.
A facet cyst appears on MRI as a fluid-filled mass near a degenerated facet joint.
Classification
Synovial facet cysts are classified by their location and associated findings:
- Lumbar cysts: Most common (especially L4–L5).
- Cervical or thoracic cysts: Rare.
- With or without nerve compression: Symptomatic (compressive) or asymptomatic (non-compressive).
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may mimic facet cyst symptoms include:
- Lumbar disc herniation
- Spinal stenosis
- Degenerative spondylolisthesis
- Epidural hematoma or abscess
- Tumors of the spine
Treatment Options
Non-Surgical Care
Most patients start with conservative management:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) reduce pain and inflammation.
- Physical therapy: Strengthening and flexibility exercises improve stability and relieve pressure.
- Heat or cold therapy: Helps reduce stiffness and discomfort.
- Epidural steroid injections: Can temporarily reduce inflammation and pain.
- CT-guided cyst rupture with steroid injection: Involves breaking the cyst and injecting anti-inflammatory medication to relieve nerve compression. Some patients may need repeat injections.
Surgical Care
Surgery is considered when symptoms persist despite conservative treatment or neurological deficits develop.
Surgical options include:
- Laminectomy and decompression: Removes part of the bone and facet joint to relieve nerve pressure and remove the cyst. Usually done for one-sided (unilateral) symptoms.
- Facetectomy with fusion: Involves removing part or all of the facet joint and stabilizing the spine with screws and rods. Indicated for:
- Bilateral or recurrent cysts
- Central spinal canal stenosis
- Instability of the vertebrae
Minimally invasive techniques allow smaller incisions, faster recovery, and less tissue disruption.
Recovery and What to Expect After Treatment
- Conservative management: Improvement may occur over several weeks or months.
- After surgery: Most patients experience immediate relief of leg pain. Hospital stays are typically 1–2 days for minimally invasive surgery.
- Rehabilitation: Physical therapy begins soon after surgery to restore movement and strengthen the back.
Full recovery usually occurs within 4–8 weeks.
Possible Risks or Side Effects (Complications)
Potential risks include:
- Recurrence of the cyst
- Nerve injury or persistent pain
- Infection or bleeding
- Spinal instability (may require fusion)
- Cerebrospinal fluid (CSF) leak
Long-Term Outlook (Prognosis)
The long-term outlook is excellent. Most patients achieve lasting pain relief and improved mobility after treatment. The recurrence rate after surgery is very low, especially when spinal stabilization is performed. Early diagnosis and treatment prevent chronic nerve compression.
Out-of-Pocket Costs
Medicare
CPT Code 63047 – Decompression / Laminectomy with Cyst Excision: $271.76
CPT Code 63005 – Limited Facet Cyst Excision: $300.40
CPT Code 22612 – Fusion (if needed): $382.85
CPT Code 22842 – Instrumentation (Rods, Screws, Plates – 3–6 Segments): $185.26
Under Medicare, 80% of the approved costs for these spine procedures are covered once your annual deductible has been met. Patients are responsible for the remaining 20%. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—usually pay this 20% portion, meaning most patients have little to no out-of-pocket costs for Medicare-approved surgeries. These supplemental policies work directly with Medicare to ensure comprehensive coverage for spinal decompression and stabilization procedures like laminectomy, cyst excision, and fusion.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare has processed the claim. After your deductible is met, the secondary plan may cover remaining coinsurance or additional costs. Secondary insurance plans typically have a modest deductible, ranging from $100 to $300 depending on the specific policy and network coverage.
Workers’ Compensation
If your lumbar facet cyst or spinal compression resulted from a workplace injury, Workers’ Compensation will cover the full cost of surgical treatment, including decompression, cyst excision, and spinal fusion if necessary. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your spinal condition or facet cyst was caused or worsened by a motor vehicle accident, No-Fault Insurance will pay for all related surgical and hospital expenses, including decompression, cyst excision, and fusion procedures. The only possible cost to you may be a small deductible depending on your policy’s terms.
Example
Patricia, a 62-year-old patient with lumbar spinal stenosis and a facet joint cyst, underwent decompression with cyst excision (CPT 63047) and posterior fusion with instrumentation (CPT 22612 + 22842) to stabilize her spine. Her Medicare out-of-pocket costs were $271.76, $382.85, and $185.26, respectively. Since she had supplemental coverage through AARP Medigap, the 20% that Medicare did not pay was fully covered, leaving her with no out-of-pocket expense for her surgery.
Frequently Asked Questions (FAQ)
Q. What causes a synovial facet cyst?
A. It develops from degenerative arthritis in the facet joints, which produces excess synovial fluid that collects and forms a cyst.
Q. How is a synovial facet cyst different from a herniated disc?
A. Both can compress nerves and cause sciatica, but a facet cyst arises from a joint, while a herniated disc comes from the intervertebral disc.
Q. Can facet cysts go away on their own?
A. Small cysts sometimes shrink or rupture naturally, but most persist or enlarge over time.
Q. When is surgery necessary?
A. Surgery is recommended for persistent pain, neurological symptoms, or spinal instability after conservative treatment fails.
Summary and Takeaway
A synovial facet cyst is a fluid-filled sac that forms due to arthritis and degeneration in the spine’s facet joints. While many cases improve with medications, therapy, or injections, surgery provides lasting relief for persistent or severe symptoms. Modern minimally invasive techniques make surgical removal safe, effective, and associated with rapid recovery.
Clinical Insight & Recent Findings
A recent case report described a 64-year-old woman with lumbar synovial facet cyst at the L4–L5 level presenting with neurogenic claudication and radicular pain after prior hip arthroplasty. MRI revealed an extradural cyst compressing the right L5 nerve root and narrowing the spinal canal.
The patient underwent posterior laminectomy, partial arthrectomy, cyst excision, and instrumented posterolateral fusion, which led to significant improvement in walking ability and only mild residual back pain two years post-surgery. The authors emphasized that lumbar facet synovial cysts, most commonly found at L4–L5 due to high mobility and facet degeneration, can mimic hip or spinal stenosis symptoms, complicating diagnosis. MRI remains the gold standard, showing well-defined, smooth, extradural lesions adjacent to facet joints.
While conservative management with analgesics, corticosteroid injections, or cyst aspiration may offer temporary relief, surgical excision combined with fusion provides the best long-term outcomes by addressing both neural compression and underlying spinal instability, thereby minimizing recurrence risk. (Study of surgical management of lumbar synovial facet cyst – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is provided by orthopedic spine surgeons or neurosurgeons, often working with pain management specialists, radiologists, and physical therapists.
When to See a Specialist?
Consult a spine specialist if you experience:
- Persistent back or leg pain
- Numbness or weakness in the legs
- Pain that worsens while standing or walking
When to Go to the Emergency Room?
Seek immediate care if you develop:
- Loss of bladder or bowel control
- Severe leg weakness or numbness
- Sudden worsening of pain after a fall or injury
What Recovery Really Looks Like?
After surgery, most patients experience immediate improvement in leg pain and mobility. Physical therapy helps strengthen the back and prevent recurrence. Return to normal activity is typically possible within 4–8 weeks.
What Happens If You Ignore It?
Ignoring a symptomatic facet cyst may lead to chronic pain, nerve damage, or worsening spinal stenosis. Early diagnosis and treatment improve outcomes.
How to Prevent It?
- Maintain good posture and spinal alignment.
- Exercise regularly to strengthen core and back muscles.
- Avoid repetitive twisting or heavy lifting.
- Manage arthritis and maintain a healthy weight.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and omega-3 fatty acids supports bone health and reduces inflammation. Staying hydrated keeps spinal joints lubricated.
Activity and Lifestyle Modifications
Engage in low-impact exercises such as swimming, yoga, or walking. Avoid high-impact activities that strain the back. Regular stretching maintains flexibility and reduces stress on the facet joints.
Do you have more questions?
What exactly is a synovial facet cyst?
A synovial facet cyst is a fluid-filled sac that develops in the facet joints of the spine due to degeneration, often causing compression of nearby nerves.
What is the difference between a synovial cyst and a ganglion cyst?
Synovial cysts are lined by a synovial membrane and contain joint fluid, whereas ganglion cysts lack this membrane and are filled with gelatinous material. Both can cause similar symptoms.
How do synovial cysts form?
These cysts form when the synovial fluid, which lubricates the joints, escapes into small tears in the joint capsule, often due to degenerative changes like osteoarthritis.
Are lumbar synovial facet cysts common?
No, they are relatively rare but are more frequently diagnosed due to advancements in imaging technologies like MRI. Posterior cysts are more common than anterior ones.
Are all lumbar synovial facet cysts symptomatic?
No, many cysts are asymptomatic and may only be discovered incidentally during imaging for other conditions.
What are the primary symptoms of a lumbar facet cyst?
Symptoms can include lower back pain, leg pain (radiculopathy), numbness, tingling, muscle weakness, and in severe cases, difficulty walking due to nerve compression.
Can a lumbar synovial cyst resolve on its own?
In some cases, small cysts may spontaneously resolve, but this is not common. Larger cysts usually require medical intervention.
What causes lumbar synovial facet cysts to grow?
They grow due to continuous degenerative changes in the spine, particularly in the facet joints, and the ongoing production of synovial fluid in response to joint irritation.
Is there a risk factor for developing these cysts?
Age, osteoarthritis, spondylolisthesis, and previous spinal trauma are significant risk factors, as these conditions contribute to joint degeneration.
How is a lumbar synovial cyst diagnosed?
The gold standard for diagnosis is MRI, which provides detailed images of the soft tissues, including cysts, and helps differentiate them from other spinal abnormalities like herniated discs.
Can lumbar synovial cysts mimic other conditions?
Yes, they can mimic conditions like disc herniations, spinal stenosis, or other nerve compressions due to similar symptoms like radiculopathy and lower back pain.
What conservative treatments are available for lumbar synovial cysts?
Conservative treatments include physical therapy, NSAIDs, corticosteroid injections, and using a back brace to reduce symptoms without surgery.
What is percutaneous aspiration or rupture of the cyst?
This is a minimally invasive procedure where a needle is guided into the cyst to either aspirate the fluid or rupture the cyst under imaging guidance, followed by a steroid injection.
Is percutaneous treatment effective?
It can be effective in the short term, but studies show that about 29% of patients need repeat procedures or further surgery because the cyst recurs or symptoms return.
When is surgery recommended for a synovial facet cyst?
Surgery is usually recommended when conservative treatments fail or if the cyst is causing significant nerve compression, leading to pain, weakness, or neurological deficits.
What is the difference between decompression surgery and decompression with fusion?
Decompression surgery removes the cyst or bone tissue compressing the nerves, while decompression with fusion involves stabilizing the spine by fusing two vertebrae together to prevent further instability.
What are the surgical options for treating lumbar synovial cysts?
Surgical options include decompression surgery, where part of the bone or tissue compressing the nerve is removed, and sometimes fusion surgery is added if there is spinal instability.
What are the risks of surgery for a lumbar synovial cyst?
Risks include infection, bleeding, spinal instability (especially if fusion is not done), and potential injury to nearby nerves or the spinal cord, though these complications are rare.
What is the recovery time after surgery for a lumbar synovial cyst?
Recovery time varies depending on the type of surgery. Decompression surgery usually involves a shorter recovery (4-6 weeks), while decompression with fusion may take several months for full recovery.
Can the cyst come back after surgery?
Recurrence is uncommon after surgical removal, particularly if fusion is also performed. However, in rare cases, cysts can form at other levels of the spine.
Is there any way to prevent synovial facet cysts from forming?
While there’s no guaranteed way to prevent these cysts, maintaining spinal health through regular exercise, a healthy weight, and avoiding heavy lifting can reduce the likelihood of degenerative changes in the spine.
What is the prognosis for patients with lumbar synovial facet cysts?
The prognosis is generally good, especially for those who undergo surgery. Most patients experience significant relief from pain and neurological symptoms.
Does the size of the cyst determine the treatment approach?
Not necessarily. Treatment is more often based on symptoms rather than cyst size. Even a small cyst can cause significant symptoms if it compresses a nerve.
What type of doctor treats lumbar synovial facet cysts?
Orthopedic surgeons or neurosurgeons specializing in spine surgery typically treat synovial facet cysts, especially when surgery is necessary. Other specialists, such as pain management doctors, may provide non-surgical treatments.
Will I need physical therapy after surgery for a synovial cyst?
Yes, physical therapy is often recommended after surgery to help restore mobility, strengthen the muscles supporting the spine, and reduce the risk of future spinal issues.

