Scoliosis is a condition in which the spine curves sideways in an abnormal “S” or “C” shape. While the spine naturally has gentle front-to-back curves that help balance weight and movement, scoliosis causes an additional side-to-side curve. This condition can occur in children, adolescents, or adults and may range from mild to severe.
In most cases, scoliosis develops gradually and is often noticed by uneven shoulders, a tilted waistline, or a leaning posture. Severe cases can cause pain, breathing difficulty, or impact internal organs if left untreated.
How Common It Is and Who Gets It? (Epidemiology)
Scoliosis affects about 2–3% of the population. It is most commonly diagnosed during childhood or adolescence—especially between ages 10 and 18. Girls are more likely than boys to develop curves that require treatment. Adults can also develop scoliosis as a result of degenerative spine changes, past untreated scoliosis, or other spinal diseases.
Why It Happens – Causes (Etiology and Pathophysiology)
Scoliosis can have different causes:
- Idiopathic scoliosis: The most common type, with no known cause. It is further divided into:
- Infantile (birth to 3 years)
- Juvenile (4–10 years)
- Adolescent (10–18 years)
- Congenital scoliosis: Caused by spinal malformations present at birth.
- Neuromuscular scoliosis: Associated with conditions like cerebral palsy, muscular dystrophy, or spinal muscular atrophy.
- Degenerative scoliosis: Occurs in adults due to age-related wear and tear on discs and joints.
- Syndromic scoliosis: Linked to syndromes such as Marfan’s or Ehlers-Danlos.
The abnormal curvature may result from asymmetrical growth of the vertebrae or muscle imbalance around the spine.
How the Body Part Normally Works? (Relevant Anatomy)
A healthy spine has three natural curves: an inward curve in the neck (cervical lordosis), an outward curve in the upper back (thoracic kyphosis), and an inward curve in the lower back (lumbar lordosis). These curves balance posture and distribute weight evenly.
In scoliosis, the vertebrae rotate and shift sideways, creating a visible deformity that may cause the ribs to protrude or the shoulders and hips to appear uneven.
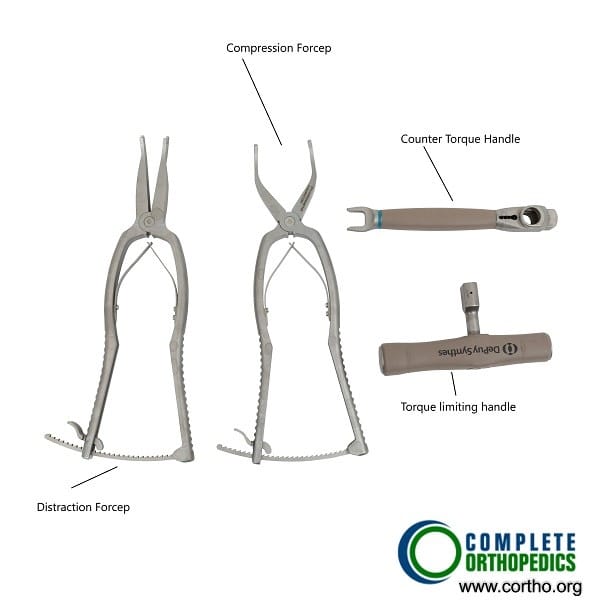
Compression and distraction instruments used in scoliosis surgery
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms depend on the severity and type of scoliosis:
- Uneven shoulders or waistline
- One shoulder blade more prominent than the other
- Rib hump when bending forward
- Tilted or leaning posture
- Back pain (more common in adults)
- Breathing difficulty in severe curves (>100°)
- Fatigue or muscle tightness in the back
Mild scoliosis often causes no pain and may only be noticed during a physical exam or school screening.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a physical examination by an orthopedic spine specialist.
- Adam’s forward bend test: Detects spinal asymmetry or rib prominence.
- X-rays: The gold standard for measuring the spinal curve using the Cobb angle.
- MRI or CT scan: May be done to evaluate spinal cord, nerves, or congenital abnormalities.
Curves greater than 10 degrees are considered scoliosis. Imaging also helps track curve progression and plan surgery if needed.
Classification
Scoliosis is classified by:
- Cause: Idiopathic, congenital, neuromuscular, degenerative, or syndromic.
- Age of onset: Infantile, juvenile, adolescent, or adult.
- Curve severity:
- Mild: <25°
- Moderate: 25–50°
- Severe: >50°
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may mimic scoliosis include:
- Postural imbalance or leg-length discrepancy
- Kyphosis (forward rounding of the spine)
- Muscle spasms from back pain
- Structural deformities due to trauma or infection
Treatment Options
Non-Surgical Care
Mild and moderate scoliosis can often be managed without surgery:
- Observation: Regular checkups every 6 months for children to monitor curve progression.
- Bracing: Prevents curve worsening in growing adolescents. Braces do not correct scoliosis but can stop progression.
- Physical therapy: Core-strengthening and posture-correction exercises improve muscle balance and reduce pain.
- Casting: Used in young children to gradually correct the curve.
Surgical Care
Surgery is recommended for severe or progressive curves (typically >50°) or when bracing fails.
Common surgical procedures include:
- Spinal fusion: The most common surgery; joins vertebrae together using rods, screws, or wires to correct and stabilize the curve.
- Growth-friendly techniques: For children, devices such as growing rods or VEPTR (vertical expandable prosthetic titanium rib) allow the spine to grow while controlling the curve.
- De-rotation or rib correction: May be performed to correct rib prominence or chest wall deformity.
Recovery and What to Expect After Treatment
- After bracing: Bracing is worn for 16–23 hours daily until growth stops. Follow-up continues with periodic imaging.
- After surgery: Hospital stay is usually 5–7 days. Most patients return to normal activities within 6–12 months. Physical therapy supports recovery and flexibility.
Modern surgical techniques have excellent success rates, improving posture and reducing pain.
Possible Risks or Side Effects (Complications)
Complications are rare but may include:
- Infection or bleeding
- Nerve injury or paralysis (very uncommon)
- Hardware failure (rods or screws)
- Lung or chest complications
- Need for revision surgery
Long-Term Outlook (Prognosis)
With proper management, scoliosis has an excellent prognosis. Children with mild curves often live normal, active lives. Surgical correction provides lasting improvement in posture, balance, and quality of life. Adults may require ongoing monitoring for degenerative changes.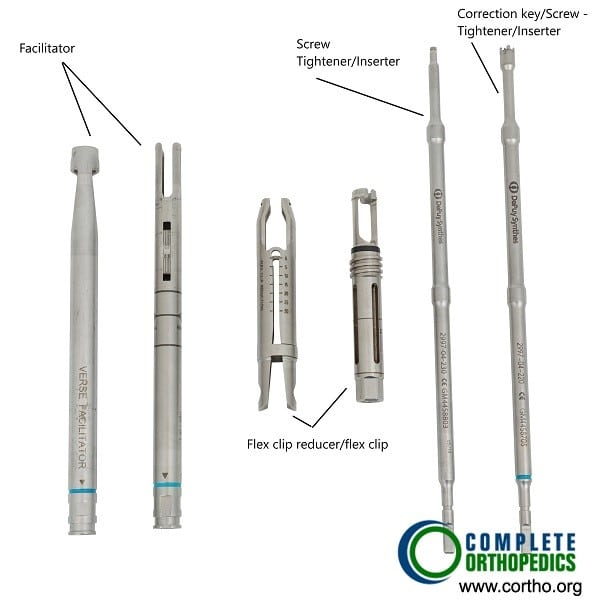
Reduction and de-rotation instruments used in Scoliosis surgery
Out-of-Pocket Cost
Medicare
CPT Code 22800 – Spinal Fusion (Posterior or Anterior Technique): $332.53
Under Medicare, 80% of the approved cost for spinal fusion is covered once your annual deductible has been met. Patients are responsible for the remaining 20%. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—typically pay this 20%, leaving most patients with no out-of-pocket expenses for Medicare-approved spinal fusion procedures. These supplemental plans are designed to work alongside Medicare, ensuring comprehensive coverage for spinal stabilization surgeries.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it functions as a secondary payer after Medicare has processed the claim. Once your deductible is satisfied, the secondary plan may cover the remaining balance, including coinsurance or small residual costs. Deductibles for secondary insurance plans typically range between $100 and $300, depending on the policy and provider network.
Workers’ Compensation
If your spinal condition or injury requiring fusion is related to a work accident, Workers’ Compensation will cover all medical and surgical expenses, including hospitalization, implants, and postoperative care. You will not have any out-of-pocket costs under an approved Workers’ Compensation claim.
No-Fault Insurance
If your spine injury or instability occurred due to a motor vehicle accident, No-Fault Insurance will cover all necessary surgical and hospital costs for spinal fusion. The only potential out-of-pocket cost is a small deductible, depending on your specific insurance policy terms.
Example
Jennifer, a 68-year-old patient with severe spinal instability, underwent spinal fusion (CPT 22800) for stabilization and pain relief. Her estimated Medicare out-of-pocket cost was $332.53. Because she had supplemental insurance through Blue Cross Blue Shield, the remaining 20% not covered by Medicare was fully paid, leaving her with no out-of-pocket expense for the surgery.
Frequently Asked Questions (FAQ)
Q. What causes scoliosis?
A. The most common type, idiopathic scoliosis, has no known cause. Other types may result from birth defects, neuromuscular conditions, or degenerative changes.
Q. Can scoliosis be cured without surgery?
A. Mild scoliosis can often be managed with observation and bracing. Surgery is only needed if the curve progresses or causes pain or breathing difficulty.
Q. Does scoliosis cause pain?
A. Mild scoliosis rarely causes pain. Severe or degenerative scoliosis may cause back pain, stiffness, or muscle fatigue.
Q. What is the recovery time after scoliosis surgery?
A. Most patients return to light activities within 6 weeks and normal activity within 6–12 months.
Summary and Takeaway
Scoliosis is an abnormal sideways curvature of the spine that can affect children and adults. Mild cases often require observation or bracing, while severe or progressive curves may need surgical correction. Modern surgical techniques provide excellent results, improving posture, balance, and overall quality of life.
Clinical Insight & Recent Findings
A recent review in the North American Spine Society Journal highlighted major advances in understanding the genetics and pathogenesis of scoliosis, which affects 2–3% of the population. The study distinguished between idiopathic scoliosis, driven largely by genetic and developmental factors, and adult degenerative scoliosis, linked to age-related spinal changes.
Idiopathic scoliosis was associated with genes such as COL11A2, GPR126, and PAX1, influencing vertebral structure, while hormonal and neural genes like ESR1, CALM1, and MTNR1B explained its higher prevalence in adolescent females. Pathophysiologic mechanisms include asymmetric cartilage growth, melatonin receptor dysfunction, and altered bone metabolism. In contrast, adult degenerative scoliosis arises from asymmetric disc and facet degeneration mediated by genes such as COX2, IL6, and COL2A1, which promote inflammation and tissue breakdown.
The authors proposed that scoliosis develops through a multifactorial interaction of genetic susceptibility, hormonal influences, and environmental stress, underscoring the need for genomic and biomechanical integration to improve early diagnosis and personalized treatment. (Study of genetics and pathogenesis of scoliosis – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Scoliosis care is managed by orthopedic spine surgeons and pediatric orthopedic specialists, supported by physical therapists, rehabilitation specialists, and pulmonary experts for severe thoracic curves.
When to See a Specialist?
You should see a specialist if you notice:
- Uneven shoulders or hips
- Visible spinal curvature
- Persistent back pain or stiffness
- Difficulty breathing with known spinal deformity
When to Go to the Emergency Room?
Emergency care is rarely required but should be sought for:
- Sudden severe back pain after trauma
- Numbness or weakness in the legs
- Difficulty breathing due to severe spinal curvature
What Recovery Really Looks Like?
Recovery is gradual but steady. Patients regain mobility and improved posture over several months. Children return to sports and normal activities once healing is complete and fusion is stable.
What Happens If You Ignore It?
Untreated scoliosis can worsen over time, leading to pain, deformity, or lung and heart complications. Early diagnosis ensures effective treatment and prevents permanent changes.
How to Prevent It?
While most scoliosis cannot be prevented, early detection through school screenings and regular checkups allows timely management and avoids progression.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and protein supports bone health and spinal strength. Maintaining healthy weight reduces back strain and enhances posture.
Activity and Lifestyle Modifications
Encourage low-impact activities such as swimming, yoga, or cycling to keep the spine flexible. Avoid heavy lifting or asymmetric sports if scoliosis is present. Practice good posture and core strengthening exercises.
Do you have more questions?
What is the main cause of scoliosis?
Most cases of scoliosis are idiopathic, meaning there is no known cause. It often appears during adolescence, particularly in girls. However, congenital, neuromuscular, and syndromic forms have specific causes like abnormal vertebral formation or underlying neurological conditions.
How is scoliosis diagnosed?
Diagnosis begins with a physical examination, including the forward bending test. If scoliosis is suspected, X-rays are used to measure the degree of the spinal curvature. Additional tests, like MRIs, may be performed in more complex cases to rule out neurological causes.
Can scoliosis be prevented?
Idiopathic scoliosis cannot be prevented since its cause is unknown. Congenital scoliosis, which occurs due to spine malformations at birth, is also not preventable. Preventive strategies are not applicable for the majority of scoliosis types.
What are the risks if scoliosis is left untreated?
If untreated, curves greater than 50 degrees often continue to worsen, potentially leading to severe spinal deformities, chronic pain, and in rare cases, cardiopulmonary complications if the curve impinges on the lungs and heart.
What is the difference between structural and non-structural scoliosis?
Structural scoliosis involves a permanent curve with vertebral rotation, often requiring treatment. Non-structural scoliosis, or functional scoliosis, is a temporary curve without vertebral rotation and is often caused by factors like muscle spasms or differences in leg length.
What is the typical age when scoliosis develops?
Idiopathic scoliosis typically develops during adolescence, between the ages of 10 and 15, coinciding with growth spurts. However, congenital scoliosis is present at birth, and neuromuscular scoliosis can develop at any age depending on the underlying condition.
How often does scoliosis progress into adulthood?
Curves less than 30 degrees typically do not progress into adulthood after skeletal maturity. However, curves greater than 50 degrees tend to progress by about 1 degree per year, even after growth has stopped.
How does scoliosis affect physical activity?
Most individuals with mild to moderate scoliosis can engage in normal physical activity without restrictions. For severe cases, activities involving excessive twisting of the spine may need to be limited. Post-surgery, patients are often advised to avoid high-impact activities for a period to allow the spine to heal.
Can scoliosis cause back pain?
While back pain is not a common presenting symptom of idiopathic scoliosis, about 25% of adolescents with scoliosis report some back pain. Severe cases, or scoliosis related to other conditions, may cause significant pain due to muscle imbalances or nerve compression.
Is scoliosis hereditary?
Yes, there is a genetic component to scoliosis. Children and siblings of patients with idiopathic scoliosis have a higher likelihood of developing the condition. However, scoliosis does not follow a simple pattern of inheritance, and other factors likely play a role.
At what point is surgery recommended for scoliosis?
Surgery is generally recommended for curves greater than 45-50 degrees in growing patients or for curves that continue to progress after skeletal maturity. It is also considered when the patient experiences significant discomfort or deformity that affects daily activities.
Will bracing correct scoliosis?
Bracing does not correct scoliosis but is intended to prevent the curve from worsening during growth. It is most effective for curves between 25 and 40 degrees in growing children. Compliance with wearing the brace is crucial for its success.
What does scoliosis surgery involve?
The most common surgery for scoliosis is spinal fusion, which involves correcting the curve using rods, hooks, screws, and wires, then fusing the vertebrae with bone grafts. This procedure stabilizes the spine and prevents further progression of the curve.
Are there risks associated with scoliosis surgery?
As with any major surgery, there are risks, including infection, bleeding, nerve damage, or complications related to the anesthesia. However, advancements in surgical techniques have significantly improved safety and outcomes.
Can adults with scoliosis still be treated?
Yes, adults with scoliosis can be treated, although treatment options differ from those for children. Pain management, physical therapy, and in some cases, surgery may be considered. Surgical correction in adults can improve symptoms but may not achieve the same level of curve correction as in children.
Can scoliosis cause respiratory or heart problems?
Severe scoliosis (usually curves greater than 90 degrees) can impact the chest cavity, restricting lung function and, in rare cases, putting pressure on the heart. This is more likely to occur if scoliosis is left untreated and allowed to progress.
What happens if scoliosis is detected after the child has stopped growing?
If scoliosis is detected after skeletal maturity, treatment options like bracing are no longer effective. Observation and periodic monitoring are used for smaller curves, while surgery may be considered for larger curves or if symptoms such as pain develop.
Is scoliosis screening necessary for children?
Screening programs for scoliosis, such as school-based screenings, are debated. Some organizations recommend routine screening for children between 10 and 14 years, while others argue that the benefits of routine screening are unclear, as it may lead to overdiagnosis.
Will scoliosis limit career choices?
For most individuals, scoliosis does not limit career choices or everyday activities. However, those with severe scoliosis, or who have undergone spinal surgery, may need to avoid careers that involve heavy lifting or physical strain on the back.
How can a parent help their child manage scoliosis?
Parents can help by ensuring their child attends regular medical check-ups, adheres to bracing schedules, and maintains a healthy lifestyle that includes physical activity. Providing emotional support is equally important, especially if the child is struggling with body image concerns.
Can scoliosis recur after surgery?
Once the spine has been fused during surgery, the area is stabilized, and the curve should not progress further. However, in rare cases, complications can occur that may require additional surgery, such as rod breakage or failure of the fusion to take hold.
Can scoliosis lead to arthritis?
Severe scoliosis can contribute to the early development of degenerative changes or arthritis in the spine due to abnormal wear and tear on the joints. This is more common in adults with untreated scoliosis.
How effective is physical therapy for scoliosis?
Physical therapy is generally used as an adjunct to other treatments for scoliosis, particularly for pain relief and improving flexibility. However, it is not a cure for scoliosis. Therapy can help improve posture and strengthen the muscles supporting the spine.
Is scoliosis painful for most patients?
Mild to moderate scoliosis is often painless and may not cause symptoms. However, more severe cases can cause discomfort, particularly in the lower back, and may lead to muscle fatigue. Postural imbalances due to scoliosis can also lead to pain over time.
What lifestyle changes can help manage scoliosis symptoms?
Staying physically active, maintaining good posture, and managing body weight can help alleviate symptoms of scoliosis. In some cases, modifications to workspaces and daily habits may reduce strain on the back.

