Atlantoaxial instability, a condition involving the destabilization of the C1-C2 segment of the cervical spine, can result from factors like odontoid fractures, arthritis, and cervical tumors. If left untreated, this instability can cause abnormal movement of the vertebrae, leading to neck pain, difficulty with movement, and an increased risk of spinal cord compression. Surgical stabilization of the atlantoaxial joint is crucial to prevent these issues and improve patient outcomes.
How Common It Is and Who Gets It? (Epidemiology)
Atlantoaxial instability is relatively rare but can occur due to trauma, degenerative disease, or congenital conditions. It is often diagnosed in patients with cervical spine fractures, severe arthritis, or spinal tumors. Treatment typically occurs when conservative methods fail to relieve symptoms, or if there is a significant risk of neurological deficits.
Why It Happens – Causes (Etiology and Pathophysiology)
The most common causes of atlantoaxial instability are:
- Odontoid Fractures: Damage to the odontoid process (the peg-like structure on the second cervical vertebra) that can destabilize the cervical spine.
- Arthritis: Degenerative arthritis, such as rheumatoid arthritis, can weaken the joints and ligaments, leading to instability.
- Cervical Tumors: Tumors in the cervical spine can cause structural damage and instability.
- Congenital Defects: Some individuals may be born with abnormalities that predispose them to atlantoaxial instability.
In these conditions, the abnormal movement of the C1 and C2 vertebrae can compress the spinal cord, leading to pain, weakness, and potential neurological impairment.
How the Body Part Normally Works? (Relevant Anatomy)
The cervical spine consists of seven vertebrae, with the first two vertebrae (C1 and C2) playing a critical role in head movement and stability. The C1 vertebra, also called the atlas, supports the skull, while the C2 vertebra (axis) allows rotation of the head. The atlantoaxial joint is formed by the articulation of the atlas and axis, with ligaments and bones maintaining the alignment and stability of the cervical spine. Any damage to these structures can disrupt spinal function and cause instability.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of atlantoaxial instability can include:
- Neck Pain: Often associated with limited range of motion.
- Headaches: Often originating from the base of the skull.
- Weakness: In the arms or legs, often indicating spinal cord compression.
- Numbness: In the arms, hands, or other extremities.
- Bowel or Bladder Incontinence: In severe cases, due to spinal cord compression.
- Loss of Balance: Difficulty walking or maintaining balance, indicating neurological involvement.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis is typically made through a combination of clinical examination and imaging studies:
- X-rays: Can show alignment issues and help identify instability.
- MRI: Provides detailed images of soft tissue, including the spinal cord and ligaments.
- CT scans: Useful for evaluating bone structures and detecting fractures or tumors.
- Fluoroscopy: During surgery, this real-time imaging can assist with screw placement and verify that the vertebrae are aligned.
Classification
Atlantoaxial instability is classified based on its underlying cause and the extent of instability:
- Odontoid Fractures: Fractures of the odontoid process that cause instability.
- Degenerative Arthritis: Arthritis affecting the C1-C2 joints, leading to instability.
- Traumatic Injuries: Dislocations or fractures resulting from trauma to the neck.
- Tumors or Infections: That disrupt normal alignment and stability.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions such as cervical spondylosis, cervical herniated discs, or myelopathy can produce similar symptoms, such as neck pain and neurological deficits. Accurate diagnosis is necessary to distinguish atlantoaxial instability from these other conditions.
Treatment Options
- Non-Surgical Care: For mild cases, physical therapy, pain management, and cervical collars may be used to manage symptoms.
- Surgical Care: If non-surgical treatments fail or if the condition worsens, surgical options include:
- Atlantoaxial Transarticular Screw (TAS): A technique to stabilize the C1-C2 joint using screws placed through the atlantoaxial joint.
- Screw and Rod Construct (SRC): A more comprehensive method involving screws and rods to stabilize the cervical spine.
Recovery and What to Expect After Treatment
Post-surgery recovery varies, but most patients can expect to stay in the hospital for a few days. After surgery, physical therapy is often needed to restore mobility and strength. The recovery process may take several weeks to months, with activity restrictions such as avoiding heavy lifting and strenuous movement. Full recovery is usually achieved within 3 to 6 months.
Possible Risks or Side Effects (Complications)
As with any spinal surgery, atlantoaxial stabilization carries certain risks:
- Infection: Infection at the surgical site.
- Nerve Injury: Damage to nearby nerves during surgery, leading to neurological deficits.
- Vertebral Artery Injury (VAI): If the screws are misaligned, the vertebral artery may be damaged.
- Hardware Failure: The screws or rods may shift or break, requiring further intervention.
- Blood Loss: Significant blood loss can occur, especially with larger incisions or complex procedures.
Long-Term Outlook (Prognosis)
The long-term outlook for atlantoaxial instability is generally good, especially with timely surgical intervention. The majority of patients experience significant relief from symptoms and can return to normal activities. However, complete recovery can take several months, and proper rehabilitation is essential for optimal outcomes.
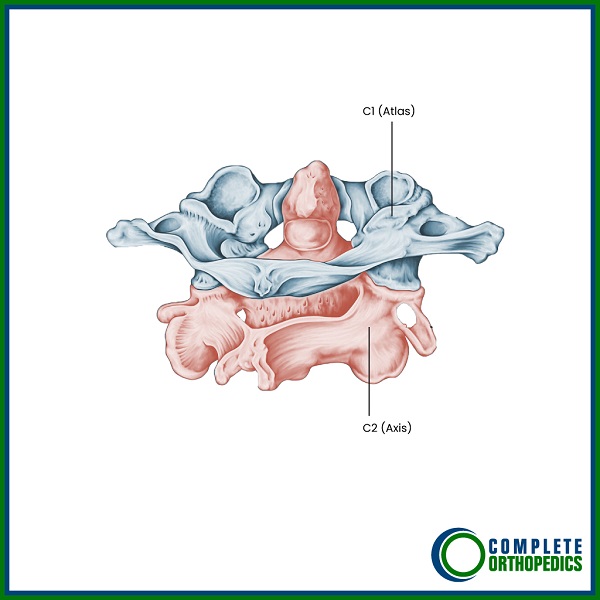
C1-C2 Facet Joint Illustrated
Out-of-Pocket Cost
Medicare
CPT Code 63020 – Posterior C1–C2 Fusion with Fluoroscopy: $378.74
Under Medicare, 80% of the approved cost for this procedure is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—generally cover this 20%, meaning most patients will have little to no out-of-pocket expenses for Medicare-approved spinal surgeries like posterior C1–C2 fusion. These supplemental plans coordinate directly with Medicare to provide full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it functions as a secondary payer once Medicare has processed the claim. After your deductible is satisfied, the secondary plan may cover any remaining balance, including coinsurance or any uncovered charges. Most secondary plans carry a modest deductible, typically between $100 and $300, depending on the policy and network status.
Workers’ Compensation
If your cervical spine condition requiring fusion resulted from a work-related injury, Workers’ Compensation will cover all related medical and surgical costs, including surgery, imaging, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your cervical spine injury resulting in C1–C2 fusion was caused by a motor vehicle accident, No-Fault Insurance will pay for all medical and surgical costs, including fusion surgery and fluoroscopic guidance. The only potential out-of-pocket expense would be a small deductible depending on your specific policy terms.
Example
Elena, a 62-year-old patient with C1–C2 instability and chronic pain, required posterior C1–C2 fusion with fluoroscopy (CPT 63020). Her estimated Medicare out-of-pocket cost was $378.74. Since she had supplemental insurance through Medigap, the 20% that Medicare did not cover was fully paid, leaving her with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. How does atlantoaxial instability affect daily activities?
A. Atlantoaxial instability can cause severe neck pain, weakness, and difficulty with balance, which may interfere with everyday tasks like walking, driving, or even maintaining posture.
Q. What is the benefit of surgical stabilization over non-surgical treatments?
A. Surgery is necessary when non-surgical methods fail to relieve symptoms or when the instability threatens spinal cord function. Surgical stabilization provides long-term relief and prevents further neurological damage.
Summary and Takeaway
Atlantoaxial instability is a serious condition that can cause significant pain and neurological deficits. Surgical stabilization, using techniques like the atlantoaxial transarticular screw (TAS) and screw and rod construct (SRC), offers effective treatment. The recovery period can be lengthy, but most patients experience significant improvement in symptoms and return to daily activities within months. Early intervention is key to preventing permanent damage.
Clinical Insight & Recent Findings
A recent study evaluated the outcomes of fluoroscopy-assisted posterior C1–C2 fixation for atlantoaxial instability, comparing the use of transarticular screws (TAS) and screw-rod constructs (SRC) in a cohort of 78 patients.
The study found that both techniques resulted in significant pain relief, with cervicalgia reducing from 88% preoperatively to 26% postoperatively. Despite the minimal complication rate, the study noted a low incidence of vertebral artery injury (2.6%) and screw malposition (6.7%), highlighting the risks associated with improper screw placement.
The research confirmed that fluoroscopy-assisted surgery is a safe and effective method for stabilizing the C1–C2 segment, offering reliable outcomes and low complication rates when performed with care. (“Study of fluoroscopy-assisted posterior C1–C2 fixation – See PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Spine surgeons, including orthopedic surgeons and neurosurgeons, typically perform atlantoaxial stabilization. The surgical team may also include anesthesiologists, nurses, and rehabilitation specialists.
When to See a Specialist?
If you experience persistent neck pain, weakness, or balance issues, or if you have been diagnosed with a cervical spine condition, consult a specialist for a comprehensive evaluation.
When to Go to the Emergency Room?
Seek immediate care if you experience sudden weakness, difficulty breathing, or loss of bowel or bladder control, as these can be signs of a spinal emergency.
What Recovery Really Looks Like?
Recovery involves a gradual improvement in symptoms, with patients usually returning to daily activities within a few months. Rehabilitation, including physical therapy, is essential for restoring strength and mobility.
What Happens If You Ignore It?
Ignoring atlantoaxial instability can lead to worsening symptoms, including paralysis or permanent loss of function. Early surgical intervention helps to prevent further damage and improve long-term outcomes.
How to Prevent It?
Maintaining good posture, avoiding neck strain, and staying active with regular exercises can help prevent cervical spine problems. Regular check-ups with a healthcare provider can also help detect early signs of instability before it requires surgery.
Nutrition and Bone or Joint Health
A diet rich in calcium and vitamin D is important for maintaining healthy bones, which support the spine. Adequate nutrition can help prevent degenerative conditions and promote healing after surgery.
Activity and Lifestyle Modifications
After surgery, patients should focus on gentle exercises that improve neck mobility and strength. It’s important to avoid heavy lifting and high-impact activities until fully recovered to ensure proper healing.
Do you have more questions?
What are the primary causes of Atlantoaxial Instability?
Odontoid fractures, arthritis, and cervical tumors are the primary causes of Atlantoaxial Instability.
What are the consequences of untreated Atlantoaxial Instability?
Untreated Atlantoaxial Instability can lead to abnormal translational and rotational movements, resulting in neck pain and an increased risk of spinal cord compression.
What surgical techniques are used to achieve atlantoaxial stability?
The atlantoaxial transarticular screw (TAS) technique and the screw and rod construct (SRC) technique are used to achieve atlantoaxial stability.
What are the risks associated with TAS and SRC procedures?
What are the risks associated with TAS and SRC procedures?
Why has the adoption of navigated surgery been slower for spine surgery compared to cranial surgery?
The setup of spinal navigation devices is relatively complex and time-consuming, contributing to slower adoption.
Is non-navigated posterior C1-C2 fixation effective in treating cervical instability and pain?
Yes, non-navigated posterior C1-C2 fixation, employing both TAS and SRC, has been proven effective.
How does the median operating room time compare between TAS and SRC techniques?
The median operating room time for SRC may be slightly longer than that of TAS, although this can vary based on user experience and surgical technique.
Which technique typically results in less blood loss, TAS or SRC?
The TAS technique typically results in less blood loss compared to the SRC technique.
What is a major complication associated with screw malpositioning in TAS and SRC procedures?
Vertebral artery injury (VAI) is a major complication, though its occurrence is very low.
What factors contribute to variations in blood loss during these surgeries?
Blood loss can be influenced by the harm caused to the venous plexuses during dissection for C1 screw placement and the use of navigation technology, which can reduce handling near the cervical venous plexuses.
How does the initial position of the screw affect the precision of C1 screw placement?
Changes in the initial screw position can affect the precision of C1 screw placement.
How can the precision of screw placement be assessed postoperatively?
Precision can be assessed using postoperative CT scans.
What is the benefit of sacrificing the C2 nerve root during these procedures?
Sacrificing the C2 nerve root can lead to fewer screw misplacements.
What is the role of surgical navigation in preventing complications during cervical spine surgery?
Surgical navigation helps prevent complications like vertebral artery injury (VAI) by improving screw precision.
Can surgical navigation entirely eliminate the risk of vertebral artery injury?
No, surgical navigation cannot entirely eliminate the risk but has shown advancements in screw precision compared to non-navigated procedures.
What other techniques can help prevent vertebral artery injury during surgery?
Techniques include the use of probing technologies based on doppler, impedance, or optical properties.
How is doppler probing utilized during C1-C2 surgical procedures?
Doppler probing is conducted during lateral dissection and stepwise drilling and tapping to prevent vertebral artery injury.
What is the Pediguard, and how is it used in spine surgery?
The Pediguard is an electronic conductivity device that aids in the placement of pedicle screws and has been used in fluoroscopy-assisted cadaveric procedures to prevent vertebral artery injury.
What is Diffuse Reflectance Spectroscopy, and how does it aid in surgery?
Diffuse Reflectance Spectroscopy is an optical technique incorporated into surgical devices to identify potential cortical breach during the insertion of pedicle screws.
What is the potential impact of integrating supportive technologies in spinal surgeries?
Supportive technologies can enhance the safety of spinal surgeries involving instrumentation.
What is the effectiveness of posterior stabilization of C1-C2 using TAS and SRC techniques?
Posterior stabilization using TAS and SRC techniques is secure and efficient, typically resulting in pain relief.
What should experienced surgeons consider until supportive technologies are widely implemented?
Experienced surgeons may consider non-navigated C1-C2 fixation as a viable choice for stabilizing the atlantoaxial segment.
What role does surgical experience play in the effectiveness of TAS and SRC techniques?
Surgical experience significantly influences the effectiveness and efficiency of TAS and SRC techniques.
What advancements have been made in screw precision for cervical spine surgery?
Advancements include the use of surgical navigation and probing technologies that improve the precision and safety of screw placement.
What are the benefits of minimally invasive approaches in these procedures?
Minimally invasive approaches, like TAS, often result in less blood loss and reduced handling near critical structures.

