Hip pain is a common problem that can result from many different causes, both within and outside the hip joint. The pain may come from conditions affecting the bones, joints, tendons, or muscles around the hip, or from referred pain originating in the spine, pelvis, or abdomen. Understanding where the pain comes from and what it feels like helps doctors determine the true source and provide effective treatment.
How Common It Is and Who Gets It? (Epidemiology)
Hip pain affects people of all ages but is most common among adults and older individuals. Athletes and people who perform repetitive movements involving the hips are more likely to develop soft-tissue causes such as bursitis or impingement. In older adults, arthritis and degenerative joint conditions are the most frequent causes. Women are slightly more prone to hip bursitis and tendinitis, while men may be more likely to develop sports-related hernias or impingement.
Why It Happens – Causes (Etiology and Pathophysiology)
Hip pain may stem from one or several underlying problems:
- Musculoskeletal causes: arthritis, tendonitis, bursitis, hip impingement, or muscle strain.
- Intra-abdominal or pelvic causes: hernias (such as inguinal or sportsman’s hernia), or gynecologic and urinary issues.
- Neurological causes: nerve compression or referred pain from the lower back.
- Systemic conditions: complex regional pain syndrome or fibromyalgia, where widespread pain and sensitivity affect multiple regions.
The specific cause determines where the pain is felt and how it behaves—sharp, dull, constant, or activity-related.
How the Body Part Normally Works? (Relevant Anatomy)
The hip is a ball-and-socket joint formed by the femoral head (ball) and the acetabulum (socket) of the pelvis. It is surrounded by strong muscles, tendons, and ligaments that provide stability and movement. Bursae cushion the joint, while cartilage allows smooth motion. Nearby nerves and blood vessels supply sensation and nutrition to the area. Proper balance among these structures is essential for pain-free walking, running, and bending.
What You Might Feel – Symptoms (Clinical Presentation)
The nature and location of hip pain vary with the cause:
- Pain on the side of the hip may suggest bursitis or tendonitis.
- Pain in the groin area often points to arthritis, impingement, or iliopsoas bursitis.
- Pain in the buttock or thigh may be referred from the lower back or sacroiliac joint.
The pain may worsen with walking, climbing stairs, or prolonged sitting. Stiffness, swelling, or clicking sensations may also occur. Persistent or worsening pain should be evaluated promptly.
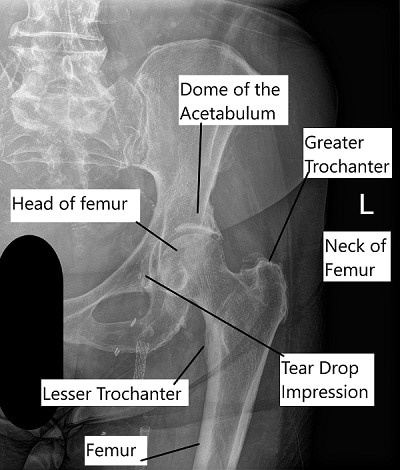
X-ray showing hip anatomy.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a detailed history and physical examination. Your doctor will ask about when the pain started, where it is located, and what makes it better or worse. The exam includes checking hip motion, gait, and special maneuvers that help identify the cause. Imaging may include:
- X-rays to look for arthritis or fractures.
- MRI or CT scans to assess soft tissue, cartilage, or labral tears.
- Ultrasound to evaluate bursitis or guide injections.
Blood tests may be ordered if infection or inflammation is suspected.
Classification
Hip pain can be broadly classified by its source:
- Intra-articular: originating from inside the joint (e.g., arthritis, labral tear, impingement).
- Extra-articular: from structures outside the joint (e.g., bursitis, tendonitis, or muscle strain).
- Referred pain: pain that originates in another region such as the spine or abdomen but is felt in the hip.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that mimic hip pain include lower back disorders, sacroiliac joint dysfunction, pelvic or abdominal hernias, and nerve entrapments. Additionally, knee arthritis or femoral stress fractures may also cause pain that radiates to the hip area.
Treatment Options
Non-Surgical Care – The first step involves rest and temporary reduction of activities that aggravate pain. Over-the-counter medications such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) help relieve pain and inflammation. Physical therapy strengthens surrounding muscles, improves flexibility, and corrects gait issues.
Surgical Care – If pain persists, targeted procedures may be recommended depending on the cause:
- Injections of corticosteroid or anesthetic for inflammation and pain control.
- Hip arthroscopy to treat labral tears or impingement in younger patients.
- Pelvic osteotomy to realign the hip joint and preserve cartilage.
- Hip replacement when severe arthritis has destroyed joint surfaces.
Recovery and What to Expect After Treatment
Recovery depends on the underlying cause and treatment method. Many patients improve with rest, medication, and therapy within a few weeks. After surgery, physical therapy plays a central role in restoring motion and strength. Most individuals return to normal daily activities within a few months, though full recovery may take longer for major procedures.
Possible Risks or Side Effects (Complications)
Possible risks include persistent pain, stiffness, infection, blood clots, or complications from surgery. Overuse of pain medications can cause stomach irritation or kidney problems. Following medical advice and rehabilitation plans minimizes these risks.
Long-Term Outlook (Prognosis)
With proper diagnosis and treatment, most people recover well from hip pain. The prognosis depends on the cause and patient factors such as age, overall health, and adherence to therapy. Chronic or degenerative conditions may require ongoing management but can still achieve good pain control and function.
Out-of-Pocket Costs
Medicare
CPT Code 20610 – Corticosteroid/Anesthetic Injection (Injection into Hip Joint or Bursa): $15.12
CPT Code 29916 – Hip Arthroscopy with Labral Repair: $240.15
CPT Code 29914 – Hip Arthroscopy for FAI (Cam Lesion Femoroplasty): $235.30
CPT Code 29915 – Hip Arthroscopy for FAI (Pincer Lesion Acetabuloplasty): $239.88
CPT Code 27146 – Pelvic Osteotomy (Realignment for Dysplasia or Impingement): $302.98
CPT Code 27130 – Total Hip Replacement (Total Hip Arthroplasty): $303.45
CPT Code 27125 – Partial Hip Replacement (Hemiarthroplasty): $268.14
Medicare Part B typically covers 80% of the approved cost for these procedures after your annual deductible has been met, leaving you responsible for the remaining 20%. Supplemental Insurance plans such as Medigap, AARP, or Blue Cross Blue Shield generally cover that remaining 20%, minimizing or eliminating out-of-pocket expenses for Medicare-approved surgeries. These plans coordinate with Medicare to fill the coverage gap and reduce financial responsibility.
If you have Secondary Insurance, such as TRICARE, an Employer-Based Plan, or Veterans Health Administration coverage, it acts as a secondary payer. These plans usually cover any remaining balance, including coinsurance or small deductibles, which typically range from $100 to $300, depending on your plan and provider network.
Workers’ Compensation
If your hip injury or degeneration requiring any of these procedures is work-related, Workers’ Compensation will cover all associated medical expenses, including surgery, injections, rehabilitation, and follow-up care. You will not have any out-of-pocket costs, as the employer’s insurance carrier directly pays for all approved treatments.
No-Fault Insurance
If your hip injury or degenerative condition is related to an automobile accident, No-Fault Insurance will typically cover the entire cost of your treatment, including arthroscopy or joint replacement. The only possible out-of-pocket cost may be a small deductible or co-payment depending on your insurance policy.
Example
Daniel Harris had persistent hip pain from impingement and underwent hip arthroscopy with labral repair (CPT 29916). His estimated Medicare out-of-pocket cost was $240.15. Later, due to worsening arthritis, he required a total hip replacement (CPT 27130) with an estimated cost of $303.45. Because Daniel had supplemental insurance through AARP Medigap, both procedures were fully covered, leaving him with no out-of-pocket expenses.
Frequently Asked Questions (FAQ)
Q. When should I see a doctor for hip pain?
A. If your hip pain lasts more than a week, limits your movement, or interferes with sleep, seek medical evaluation.
Q. Can hip pain go away on its own?
A. Minor strains may improve with rest and over-the-counter pain relief, but persistent or worsening pain needs professional assessment.
Q. Is hip pain always from arthritis?
A. No. Many cases come from soft tissue irritation, bursitis, or even spinal problems. A thorough evaluation helps identify the true cause.
Summary and Takeaway
Hip pain can result from a wide range of conditions—from muscle strain and bursitis to arthritis and impingement. Accurate diagnosis through examination and imaging ensures the right treatment, which may include rest, medication, therapy, or surgery. Early evaluation is key to effective relief and long-term joint health.
Clinical Insight & Recent Findings
A recent study explores the effectiveness of hip pericapsular nerve blocks (hip-PNB) for managing pain following total hip arthroplasty (THA). This approach combines anterior and posterior nerve blocks, addressing both the front and back of the hip joint to reduce pain more effectively than traditional methods.
The study demonstrated that using hip-PNB as part of multimodal analgesia can reduce opioid consumption, improve recovery, and alleviate pain faster compared to standard treatments.
However, further research is needed to determine the independent benefits of the posterior pericapsular deep gluteal block (PPD) when combined with the pericapsular nerve group (PENG) block. This research highlights the potential for better pain management strategies for patients undergoing hip surgery. (“Study on improving postoperative pain management in hip replacement surgery – see PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic surgeons, sports medicine physicians, and physiatrists commonly manage hip pain. Radiologists may assist with diagnostic imaging and guided injections. Physical therapists play an essential role in recovery and long-term rehabilitation.
When to See a Specialist?
If your hip pain persists beyond two weeks, interferes with walking, or is accompanied by stiffness, swelling, or clicking, it’s time to see a specialist. Prompt evaluation helps prevent chronic problems.
When to Go to the Emergency Room?
Go to the emergency room for severe hip pain after a fall or injury, inability to bear weight, visible deformity, or signs of infection such as redness, swelling, or fever.
What Recovery Really Looks Like?
Recovery may involve a short period of rest followed by physical therapy. Improvement is gradual as strength and flexibility return. For surgical patients, full recovery can take several months with progressive therapy and activity resumption.
What Happens If You Ignore It?
Ignoring hip pain can lead to worsening stiffness, chronic inflammation, and reduced mobility. Untreated conditions like arthritis or impingement may cause permanent damage to the joint cartilage, requiring more extensive surgery later.
How to Prevent It?
Prevention includes maintaining a healthy weight, warming up before activity, stretching hip and leg muscles, and using proper form during exercise. Avoid repetitive stress and manage early pain before it worsens.
Nutrition and Bone or Joint Health
A diet high in calcium, vitamin D, and protein supports bone strength and healing. Staying hydrated and maintaining a healthy body weight reduce stress on the hip joint.
Activity and Lifestyle Modifications
Low-impact exercises such as swimming, cycling, and yoga help maintain joint flexibility without overloading the hip. Gradual return to activity after rest or injury prevents recurrence. Good posture, proper footwear, and regular stretching all support long-term hip health.
Do you have more questions?
How can I differentiate between hip pain caused by musculoskeletal issues, such as arthritis, and pain originating from intra-abdominal problems like hernias?
Distinguishing between musculoskeletal hip pain and pain originating from intra-abdominal issues can be challenging. Asking your healthcare provider about specific symptoms, such as location, severity, and exacerbating factors, may help clarify the underlying cause of your hip pain.
What lifestyle modifications can I implement to alleviate hip pain, and are there any activities I should avoid to prevent exacerbating the condition?
Making lifestyle modifications may help alleviate hip pain and improve overall joint health. Your healthcare provider can offer guidance on activities to avoid and recommend exercises or ergonomic adjustments to support hip health and minimize discomfort.
Are there any specific risk factors or predisposing factors that may increase my likelihood of experiencing hip pain, and how can I mitigate these risks?
Identifying risk factors or predisposing factors for hip pain can help you take proactive steps to mitigate these risks and prevent future episodes of discomfort. Your healthcare provider can provide personalized recommendations based on your medical history, lifestyle factors, and overall health status.
Can psychological factors, such as stress or anxiety, contribute to or exacerbate hip pain, and are there strategies for addressing these factors as part of a comprehensive treatment plan?
Psychological factors, including stress and anxiety, may contribute to or exacerbate hip pain in some individuals. Integrating strategies for addressing psychological factors, such as stress management techniques or cognitive-behavioral therapy, as part of a comprehensive treatment plan may help improve overall pain management and quality of life.
What role does posture and body mechanics play in the development and management of hip pain, and are there specific exercises or techniques to improve alignment and reduce strain on the hip joint?
Posture and body mechanics can influence the development and management of hip pain. Your healthcare provider or physical therapist can recommend exercises or techniques to improve posture, strengthen supportive muscles, and reduce strain on the hip joint, which may help alleviate discomfort and prevent further injury.
Is there a connection between hip pain and other musculoskeletal conditions, such as lower back pain or knee pain, and how can addressing underlying issues in one area of the body impact hip health?
Hip pain may be interconnected with other musculoskeletal conditions, such as lower back pain or knee pain, due to biomechanical relationships within the body. Addressing underlying issues in one area of the body, such as through physical therapy or targeted exercises, may positively impact overall hip health and reduce pain.
Are there any specific dietary supplements or nutritional interventions that may help support joint health and alleviate hip pain, and how do I ensure safe and effective use of these supplements?
Certain dietary supplements or nutritional interventions may offer benefits for joint health and pain management. Your healthcare provider or a registered dietitian can provide guidance on safe and effective use of supplements, as well as recommend dietary modifications to support overall joint health and reduce inflammation.
What role does weight management play in managing hip pain, and are there recommended weight loss strategies for individuals experiencing discomfort or limited mobility due to hip issues?
Weight management can play a significant role in managing hip pain, as excess body weight can increase stress on the hip joint and exacerbate symptoms. Your healthcare provider can offer personalized recommendations for weight loss strategies, including diet modifications, exercise programs, and lifestyle changes tailored to your individual needs and goals.
How can I best advocate for myself in seeking appropriate diagnosis and treatment for hip pain, and what steps can I take to ensure I receive comprehensive care and support throughout the treatment process?
Advocating for yourself in seeking appropriate diagnosis and treatment for hip pain involves actively participating in discussions with your healthcare provider, asking questions, expressing concerns, and seeking second opinions if necessary. Building a collaborative relationship with your healthcare team and advocating for comprehensive care can help ensure you receive the support and treatment you need for effective pain management and recovery.
Are there any alternative or complementary therapies, such as acupuncture or massage, that may help alleviate hip pain, and how do I determine if these treatments are appropriate for me?
Alternative or complementary therapies like acupuncture or massage may offer relief for some individuals with hip pain. Your healthcare provider can discuss the potential benefits and risks of these therapies, as well as help you determine if they are appropriate for your specific condition and overall health
What are the potential long-term effects of chronic hip pain, and how can I best manage and cope with ongoing discomfort to maintain quality of life?
Chronic hip pain can have significant long-term effects on quality of life, including decreased mobility, functional limitations, and psychological distress. Learning effective pain management strategies, engaging in regular physical activity, and seeking support from healthcare providers or support groups can help you cope with ongoing discomfort and maintain overall well-being.
How does aging affect the prevalence and management of hip pain, and are there age-specific considerations I should be aware of in addressing my symptoms?
Aging can impact the prevalence and management of hip pain due to factors such as degenerative changes in the joint, decreased muscle strength, and changes in activity levels. Your healthcare provider can provide age-specific recommendations and considerations for managing hip pain, taking into account your individual needs, preferences, and overall health status.
Can hip pain be a symptom of more serious underlying conditions, such as infection or cancer, and what warning signs should I watch for that may indicate the need for urgent medical attention?
Hip pain can sometimes be a symptom of more serious underlying conditions, including infection or cancer. It’s important to be aware of warning signs such as persistent pain, unexplained weight loss, fever, or changes in bowel or bladder function that may indicate the need for urgent medical attention. If you experience any concerning symptoms, seek prompt evaluation from a healthcare provider.
How does gender influence the risk of developing hip pain, and are there gender-specific factors or considerations that may impact diagnosis and treatment?
Gender may influence the risk of developing hip pain due to differences in anatomy, hormonal factors, and activity levels between males and females. Your healthcare provider can discuss gender-specific considerations and recommendations for diagnosis and treatment based on current research and clinical guidelines.
Can certain occupations or activities increase the risk of hip pain, and are there specific ergonomic modifications or preventive measures I should consider to reduce my risk of injury?
Certain occupations or activities that involve repetitive motions, heavy lifting, or prolonged periods of sitting or standing may increase the risk of hip pain and injury. Your healthcare provider or occupational therapist can offer guidance on ergonomic modifications, proper lifting techniques, and preventive measures to reduce your risk of hip pain related to occupational or recreational activities.
What role does inflammation play in the development and progression of hip pain, and are there dietary or lifestyle factors that can help reduce inflammation and alleviate symptoms?
Inflammation may contribute to the development and progression of hip pain, particularly in conditions such as arthritis or bursitis. Your healthcare provider or a registered dietitian can discuss dietary and lifestyle factors that may help reduce inflammation and alleviate symptoms, such as consuming anti-inflammatory foods, maintaining a healthy weight, and managing stress.
Are there genetic factors or hereditary conditions that may predispose me to hip pain, and how can I determine if my family history influences my risk of developing hip problems?
Genetic factors or hereditary conditions may play a role in predisposing individuals to hip pain or musculoskeletal disorders. Discussing your family history with your healthcare provider can help determine if you have any genetic predispositions or familial patterns that may influence your risk of developing hip problems, allowing for proactive management and preventive measures.
What are the potential limitations or risks associated with surgical interventions for hip pain, and how can I make an informed decision about whether surgery is the right option for me?
Surgical interventions for hip pain carry potential limitations and risks, including complications, prolonged recovery periods, and uncertain outcomes. Your healthcare provider can discuss the potential benefits and risks of surgery, as well as alternative treatment options, allowing you to make an informed decision about whether surgery is the right option for you based on your individual circumstances and treatment goals.
