Shoulder Impingement
Shoulder impingement syndrome is one of the most common cause of pain in adult shoulder. It is usually caused due to repetitive overhead activities like in racquet game players, swimmers, painters, etc. This pain may lead to some weakness also.
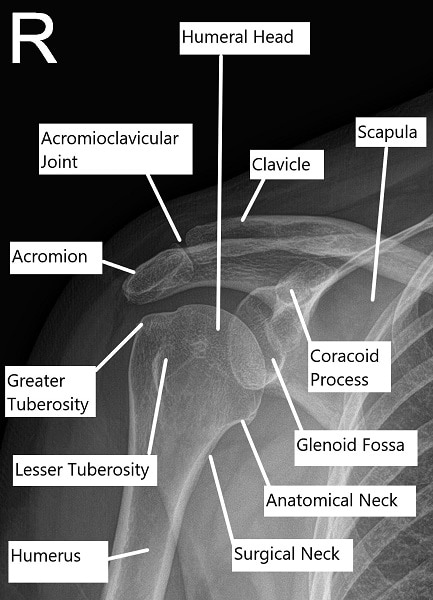
Certain tests are done in the office by the physician which help in confirmation of the diagnosis to suggest the diagnosis, confirmation of the diagnosis as well as ruling out of other conditions like rotator cuff tear can be done by performing an MRI of the shoulder joint. Bone spurs on the undersurface of the acromion and the acromioclavicular joint may dig into the rotator cuff tendon causing inflammation.
This condition is called impingement syndrome. Occasionally, patients may have impingement from the inside of the shoulder on to the rotator cuff. This condition is called internal impingement. The patients may develop irritation of the bursa along with inflammation with or without bone spurs under the acromion or the acromioclavicular joint. These patients initially present with inflammation of the rotator cuff or tendinitis and have symptoms of pain on overhead activity.
Shoulder Impingement Diagnosis
Patients with impingement syndrome most commonly present with pain in the side and front of the shoulder which is exacerbated with movement, especially overhead elevation as well as rotation. These patients may also complain of nighttime pain, discomfort and awakenings. The diagnosis of impingement syndrome is usually suggested by certain tests that are done by the physician in the office. The tear can be confirmed with the help of advanced imaging and x-rays usually performed to rule out any bony injury as well as to look for bone spurs or osteophytes which are common under the acromion and over the acromioclavicular joint. Confirmation of diagnosis as well as to rule out other diagnosis like rotator cuff tear can be done with MRI.
Shoulder Impingement Treatment
Impingement syndrome is essentially treated conservatively with the use of specific exercises, especially for the internal impingement and possible cortisone injection to decrease the inflammation along with rest and anti-inflammatory medications. If patient fails all form of conservative therapy, then surgical treatment can be offered. In case of impingement, the bone spurs need to be removed along with the excision of the inflamed bursa to decrease the pain as well as the cause of inflammation. This surgery is done arthroscopically through small incisions and is called Subacromial Decompressing (SAD) and Bursectomy. It may occasionally be associated with Distal Clavicular Excision (DCE) if there are acromioclavicular bone spurs impinging on the rotator cuff.
Following the surgery, the shoulder is immobilized in a shoulder sling and patient discharges home on the same day. The patient is instructed to gradually increase their shoulder movement overtime as much as they can do with pain tolerating. Patients are provided pain medications in the are usually discharged home after the surgery. Patients are usually seen back in the office within one week after the surgery. Recovery from surgery for impingement is quicker and patient may return to full function within 3 to 6 weeks of surgery. Physical therapy is usually not needed in most cases.
Shoulder Impingement Risks and Complications
Complications are not common but can occur. It is pertinent that patients understand prior to making the decision of have this operation so you can make an informed decision on the advantages and disadvantages of surgery. These can be:
Medical (Anesthetic) complications:
Medical complications include those due to your general wellbeing and due to Anaesthesia given before and during the surgery. These include but not limited to:
Allergic reactions to medications, excessive blood loss requiring transfusion with its low risk of disease transmission, heart attack, stroke, kidney failure, pneumonia, bladder infections. Complications from nerve blocks such as infection or nerve damage. Serious medical problems can lead to ongoing health concerns, prolonged hospitalization.
Surgical Complications:
Risks of SAD, Bursectomy with or without DCE surgery may include though not limited to:
- Infection – Patient may need to be administered prolonged antibiotics or even undergo cleaning surgery. Results are usually suboptimal in this population group.
- Stiffness – Despite physical therapy and patient motivation, stiffness may occur. It is treated with Physical therapy. Recalcitrant shoulder stiffness may require capsular release to regain range of motion.
- Instability of distal clavicle
- Tingling and numbness
- Damage to nerves or vessels
- Residual pain
- Reflex Sympathetic Dystrophy
- Some of these conditions may require hospitalization, aspiration, injections or even surgery
Certain patient population is at a higher risk for complication which include but are not limited to:
- Smoking
- Seizures
- Obstructive sleep apnea
- Obesity
- High blood pressure
- Diabetes
- Other medical conditions involving your heart, lungs or kidneys
- Medications, such as aspirin, that can increase bleeding
- History of heavy alcohol use
- Drug allergies
- History of adverse reactions to anesthesia
WHEN TO VISIT AN EMERGENCY ROOM AFTER A SURGERY:
- Suspected cardiac problem: severe chest pain or pressure, shortness of breath, tightness in chest, pain in left arm, jaw pain, dizziness or fainting, unexplained weakness or fatigue, rapid or irregular pulse, sweating, cool, clammy skin, and/or paleness
- Suspected Stroke: trouble speaking, changes in vision, confusion or other change in mental status
- Suspected venous thrombosis: swelling of the legs, ankles, or feet, discomfort, heaviness, pain, aching, throbbing, itching, or warmth in the legs, sudden shortness of breath, chest pain, coughing up blood, rapid or irregular heart rate
- Suspected Sepsis: high grade fever, with shivers associated with fatigue, dizziness, racing heart, pale or discolored skin, sleepy, difficult to rouse, confused, short of breath
- Heavy bleeding from the surgical site
- Severe allergic reaction with trouble breathing, swelling, hives
WHEN TO CONTACT A DOCTOR’S OFFICE AFTER SURGERY:
- temperature more than 101 degrees Fahrenheit
- increased pain or tenderness near the incision
- poor pain relief
- signs of infection: increased swelling, redness, increased drainage, increased warmth, pus, foul smell, bleeding at the incision, incision coming apart
- inability to feel or move fingers or toes
- pale blue, white or abnormally cold fingers or toes
- nausea (upset stomach) or vomiting (throwing up) that won’t stop
- increased tiredness
- a generally worse feeling than you had when you left the hospital
- problems urinating, severe constipation or severe diarrhea
- a concern about any other symptoms that seem unusual
SUMMARY
Impingement syndrome is common and usually present with pain and weakness in overhead activities. Physical examination as well as MRI can be helpful in diagnosis of pathology. Impingement syndrome and rotator cuff tendinitis are usually treated conservatively. Patients who fail conservative treatment may need surgical treatment in the form of arthroscopic surgery. The results of arthroscopic surgeries are good and reliable.
I am Vedant Vaksha, Fellowship trained Spine, Sports and Arthroscopic Surgeon at Complete Orthopedics. I take care of patients with ailments of the neck, back, shoulder, knee, elbow and ankle. I personally approve this content and have written most of it myself.
Please take a look at my profile page and don't hesitate to come in and talk.