The human spine is the central structural support of the body. It provides strength, stability, and flexibility while protecting the spinal cord and nerve roots. The spine is made up of five main regions: the cervical, thoracic, lumbar, sacral, and coccygeal segments. Together, these sections create the familiar double “S” curve of the vertebral column that allows upright posture and efficient weight distribution.
Functional Anatomy
The spine is composed of 33 individual bones called vertebrae, stacked one on top of another. These are grouped into regions according to their location:
- Cervical spine (neck): 7 vertebrae (C1–C7)
- Thoracic spine (mid-back): 12 vertebrae (T1–T12)
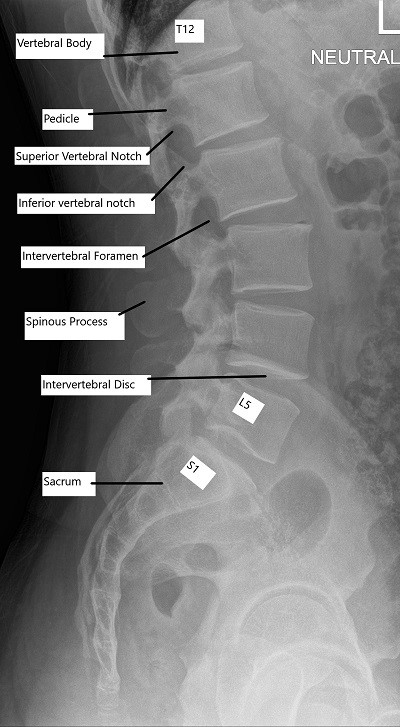
- Lumbar spine (lower back): 5 vertebrae (L1–L5)
- Sacral spine: 5 vertebrae fused into one bone
- Coccyx (tailbone): 4 fused vertebrae
Each vertebra contributes to the stability and motion of the column while forming a central canal for the spinal cord.
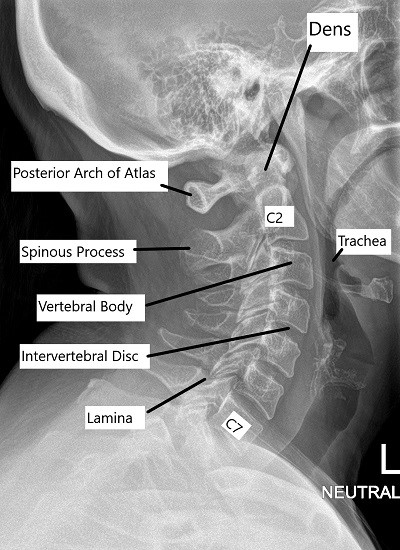
The cervical spine starts from the base of the skull and ends in the upper chest. The cervical spine helps in the movement of the head while providing stability. The thoracic spine connects the cervical spine with the lumbar spine, starting in the upper chest and ending in the mid-back.
The thoracic spine connects with the rib cage. The lumbar spine consists of large vertebrae as it supports the body weight, connecting the upper body with the pelvis.
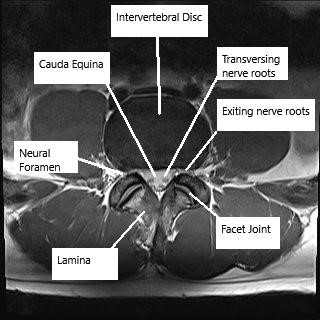
MRI showing the lumbar spine in the axial and sagittal section
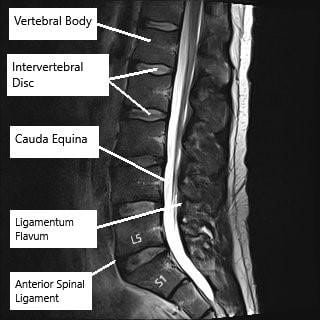
MRI showing the lumbar spine in the axial and sagittal section.
Biomechanics or Physiology
The spine’s double “S” shape is key to its function. The cervical and lumbar regions curve inward (lordosis), while the thoracic and sacral regions curve outward (kyphosis). These alternating curves act like a spring, distributing mechanical stress and maintaining balance during movement.
The spine’s flexibility allows for bending, twisting, and rotation, while its strength supports the weight of the head, arms, and torso. The intervertebral discs and facet joints work together to facilitate smooth and controlled motion.
Common Variants and Anomalies
Normal variations in spinal anatomy are common and often asymptomatic. Some people have mild differences in the shape or number of vertebrae, such as partial fusion between segments or transitional vertebrae at the lumbosacral junction. Minor curvature differences may also occur, resulting in variations of posture or spinal alignment.
Clinical Relevance
Back and neck pain are among the most frequent causes of work absenteeism and disability worldwide. Although most cases improve without surgery, some persist due to underlying conditions such as herniated discs, spinal stenosis, or facet joint arthritis.
The sciatic nerve, formed from the lower spinal roots, is commonly affected by lumbar spine disorders. Studies show that nearly 40% of adults experience sciatica during their lifetime, often due to disc herniation or foraminal narrowing.
Imaging Overview
X-rays provide basic visualization of spinal alignment and bone integrity. CT scans give detailed images of bone structures and are helpful in trauma or degenerative conditions. MRI is the best imaging tool for assessing soft tissues, including intervertebral discs, ligaments, nerve roots, and the spinal cord.
MRI can also show disc herniations, nerve compression, and postoperative changes such as the placement of a prosthetic cervical disc — an implant that restores motion at a diseased spinal segment.
Associated Conditions
Common spine-related conditions include:
- Degenerative disc disease – age-related wear of intervertebral discs.
- Herniated disc – displacement of the disc’s nucleus pulposus, compressing nerves.
- Scoliosis and kyphosis – abnormal curvature of the spine.
- Facet joint syndrome – arthritic changes in the joints connecting vertebrae.
- Spinal stenosis – narrowing of the spinal canal leading to nerve compression.
- Spondylolisthesis – forward slippage of a vertebra over the one below it.
Surgical or Diagnostic Applications
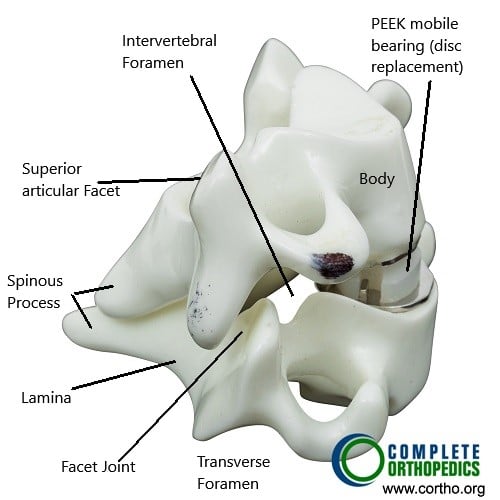
When conservative treatments fail, spinal surgery may be indicated to relieve pressure on nerves or stabilize the spine. Common procedures include discectomy, laminectomy, and spinal fusion.
In the cervical spine, artificial disc replacement can preserve motion at the affected level, offering an alternative to fusion surgery. Postoperative imaging ensures that implants are positioned correctly and spinal alignment is maintained.
Prevention and Maintenance
Maintaining spinal health involves regular physical activity, good posture, and ergonomic body mechanics. Core strengthening, stretching, and avoiding prolonged sitting reduce strain on the lower back.
Healthy weight management and proper lifting techniques also help prevent disc injuries. Early recognition and treatment of spinal conditions can prevent chronic pain and disability.
Research Spotlight
A recent study in the *Asian Spine Journal* compared lumbar spine anatomy in supine versus weight-bearing (standing) MRI to assess how spinal structures change under physiological load. The researchers analyzed 12 adults without back pain and found that nearly all measured parameters—including spinal canal width, disk height, and foraminal dimensions—changed significantly between positions.
The sagittal spinal canal diameter increased by up to 12.6% under weight-bearing, suggesting postural widening due to spinal curvature and joint adjustments. In contrast, intervertebral disk heights decreased by 3–10%, consistent with gravitational compression, while foraminal heights and cross-sectional areas generally decreased except at the L5–S1 level, which slightly expanded, likely due to sacral angle adjustment and facet joint orientation.
The intraclass correlation coefficients (ICCs) showed excellent reliability (0.75–0.98) across all measurements, confirming consistency of results. These findings demonstrate that weight-bearing MRI captures biomechanical changes in the lumbar spine that are often missed in traditional supine imaging, offering potential diagnostic value for conditions like stenosis and radiculopathy. (Study of lumbar spine morphology in supine versus weight-bearing MRI – See PubMed.)
Summary and Key Takeaways
The human spine is a dynamic structure that provides both strength and mobility. It supports the head, protects the spinal cord, and allows for a wide range of movements. Its curves and interlocking joints distribute forces efficiently and maintain balance.
Disorders of the spine can cause pain, nerve compression, or loss of function, but early diagnosis and proper care can help maintain long-term spinal health. Advances in imaging, minimally invasive surgery, and prosthetic implants continue to enhance patient recovery and preserve motion.
Do you have more questions?
Do pinched nerves go away on their own?
The pinched nerves are usually caused due to inflammation of the nerve roots near the spinal cord where they exit. The inflammation, once improved, causes relief in the pinched nerve. This improvement in inflammation can be caused rest, anti-inflammatory medication, steroid medications or cortisone shot. Occasionally the cause of inflammation may be persistent compression over the nerve, which may not get better with all form of conservative management.
What is mild back sprain, and how do you fix it?
Back sprain means injury to the ligaments or the muscles of the back. It can usually happen due to certain activity or may be with a fall or accident. The underlying cause of a back sprain may be weakening of the muscles of the back which may predispose the person to develop back sprains. If a back sprain is recurrent, then they may need physician medical attention to take care of their back so as to prevent further recurrences.An episode of back sprain can usually be treated with short term rest for one to two days along with anti-inflammatory medications and use of ice or heat to decrease the pain. This should be followed by usual activity as well as exercises involving strengthening and stretching of back muscles.
Can I jog if I have a back sprain that is hurting?
If jogging causes worsening of the back sprain, then it should better be avoided. If comfortable, one can try to do walking or fast walking too in place of jogging.
Is it best to rest for a sore back?
For a sore back or low back pain, a short term rest for one to two days may be helpful. Rest for longer periods have not been found to cause much effect in the long term and should be avoided. Prolonged rest can cause weakening of the muscles which may predispose to recurrence of back pain.
What you do for a pinched nerve in the lower back?
Most patients who have pinched nerve in the lower back present with sciatica or pain radiating down the leg. This may or may not be associated with tingling or numbness. Such patients are usually treated with medications and exercises. If the pain, tingling, and numbness are not relieved with conservative means, then these patients may need to undergo advanced imaging in the form of MRI to rule out disc disease and be treated accordingly.
What muscles are affected by the C5 and C6 nerves?
C5 and C6 nerves innervate the muscles of the shoulder and the elbow. The patients who has involvement of C5 and C6 will have pain over a shoulder and the upper arm and going up to the outer side of the forearm and the thumb. These patients may have tingling and numbness of the same area and may have weakness in the shoulder and the elbow presenting in the form of elevating the shoulder and bending the elbow.
Can you drive after back surgery?
Patients who undergo back surgery are asked not to drive until they are off pain medications as well as they are comfortably sitting in a car, in a chair for prolonged period.
What helps with neck pain?
Patients with neck pain can usually be treated with short period of rest along with antiinflammatory medications. They can also wear a soft collar if that is helpful in pain relief. Patients are encouraged to strengthen their neck muscles over a period of time with or without supervision of a physical therapist so as to treat neck pain as well as prevent recurrences.
Can exercise help neck pain?
Exercise are of tremendous help in patients with neck and back pain. They help in strengthening the muscles and thereby improving the health of the muscles. Strong muscles offload the bones of the neck and help in relieving the neck pain.
What is spondylosis of the neck?
Spondylosis is another term for degeneration or osteoarthritis of the bones of the neck. They usually present with neck pain with or without radiating pain down the arms. X-rays of the neck may show signs of osteoarthritis in the form of leaking or bone spurs.
Can a neck pain be caused by cancer?
Though a rare cause, but there is a possibility for a cause of neck pain. Any patient who has longstanding neck pain which is not relieved with conservative needs or has a history of malignancy in the past or have unintentional weight loss should seek medical attention to rule out the diagnosis.
Can a pinched nerve go away on its own?
Most of the patient’s with pinched nerve usually improves over time and pressure of the nerve is decreased due to the healing mechanism of the body. Only if the patient is not relieved of symptoms of pain, tingling or numbness, or there is worsening of symptoms and pain with or without involvement of muscles in the form of weakness or bowel or bladder, then these patients should seek medical attention.
What are the signs of pinched nerve in the neck?
Pinched nerve in the neck usually presents with radicular pain going down their arms. This may or may not be associated with tingling or numbness. If the pain is associated with weakness of the muscle, then the patient should seek urgent medical attention

