Lumbar Canal Stenosis refers to narrowing of the spinal canal in the lower back (lumbar spine). This narrowing reduces the space available for the spinal nerves, causing pressure and irritation. It can affect one or multiple levels of the spine and often leads to back pain, leg pain, numbness, or weakness.
How Common It Is and Who Gets It? (Epidemiology)
Lumbar canal stenosis is one of the most common spine problems in adults over the age of 50. It usually develops from age-related wear and tear (degeneration) of the spine. Men and women are affected equally. People with congenital (since birth) narrow canals are more likely to develop symptoms earlier.
Why It Happens – Causes (Etiology and Pathophysiology)
The most common cause is degeneration due to aging. Over time, discs lose water and height, ligaments thicken, and joints enlarge with arthritis. These changes narrow the spinal canal and put pressure on the nerve roots.
Other causes include:
- Disc herniation or bulging discs
- Bone spurs (osteophytes) from arthritis
- Thickening of the ligamentum flavum (a supporting spinal ligament)
- Congenital stenosis (narrow spinal canal at birth)
- Trauma, fractures, or dislocations
- Post-surgical or degenerative instability
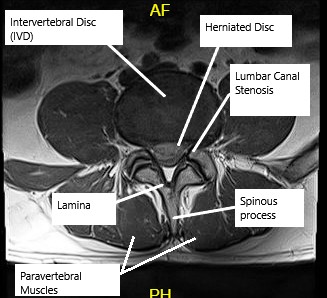
MRI showing Lumbar Canal Stenosis
How the Body Part Normally Works? (Relevant Anatomy)
The lumbar spine consists of five vertebrae connected by intervertebral discs and facet joints. These structures allow flexibility while protecting the spinal cord and nerves. The spinal canal houses the nerves that branch out to the legs. When the canal narrows, nerves become compressed, causing symptoms of pain, numbness, or weakness in the lower body.
What You Might Feel – Symptoms (Clinical Presentation)
Common symptoms include:
- Pain, tingling, or numbness in one or both legs
- Leg weakness or heaviness, especially after walking or standing
- Relief when bending forward or sitting (known as the “shopping cart sign”)
- Pain worsening when standing upright or walking downhill
- In severe cases, loss of bladder or bowel control (cauda equina syndrome, a surgical emergency)
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a detailed medical history and physical examination. Your doctor will check leg strength, sensation, and reflexes.
Imaging tests may include:
- X-rays: Show alignment and bone spurs.
- MRI: Reveals soft tissue and nerve compression.
- CT scan: Provides detailed bone structure, useful if MRI cannot be performed.
Classification
Lumbar stenosis can be classified by location and extent:
- Central stenosis: Narrowing in the middle of the spinal canal, compressing multiple nerves.
- Lateral recess stenosis: Compression of nerves as they branch out.
- Foraminal stenosis: Narrowing where nerves exit the spine.
It can also be described as single-level or multi-level based on the number of affected segments.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that can mimic lumbar canal stenosis include:
- Herniated disc
- Peripheral neuropathy (nerve disease)
- Vascular claudication (poor blood flow to legs)
- Hip or knee arthritis
- Spinal tumors or infections
Treatment Options
Non-Surgical Care
Most patients respond well to conservative treatment:
- Medications: Anti-inflammatory drugs and pain relievers.
- Physical therapy: Strengthens core and back muscles, improving flexibility and posture.
- Activity modification: Avoiding prolonged standing or heavy lifting.
- Epidural steroid injections: Reduce inflammation and relieve nerve pressure.
- Lifestyle changes: Weight management, exercise, and smoking cessation.
Surgical Care
Surgery is considered when symptoms persist despite conservative treatment or if neurological deficits worsen.
Common surgical procedures include:
- Laminectomy: Removal of the back part of the vertebra (lamina) to create space for nerves.
- Laminotomy: Partial removal of lamina for targeted decompression.
- Foraminotomy: Widening of openings (foramina) where nerves exit.
- Laminoplasty: Opening the lamina to enlarge the canal while preserving bone.
- Fusion surgery: Used when there is spinal instability, combining decompression with rods, screws, and bone grafts to stabilize the spine.
Minimally invasive techniques may be used to reduce recovery time and tissue damage.
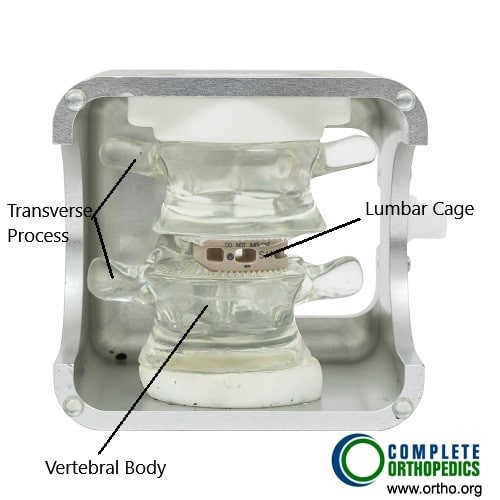
Transforaminal atraumatic lumbar interbody fusion cage
The image shows a lumbar fusion done with transforaminal technique. The fusion is aided by the bone cage which is filled with bone graft. The fusion of the segment results relief from symptoms of lumbar canal stenosis.
Recovery and What to Expect After Treatment
- Non-surgical treatment: Many patients improve within 6–12 weeks.
- After surgery: Hospital stay is typically 1–3 days. Walking is encouraged soon after surgery.
Physical therapy starts within weeks to restore strength and flexibility. Most patients experience significant pain relief and improved walking tolerance.
Possible Risks or Side Effects (Complications)
Potential risks include:
- Infection or bleeding
- Nerve or spinal cord injury
- Persistent pain or recurrence
- Dural tear causing spinal fluid leakage
- Fusion failure or hardware complications
Careful planning and adherence to post-surgical instructions minimize these risks.
Long-Term Outlook (Prognosis)
Most patients achieve excellent relief from pain and improved function after appropriate treatment. Surgery provides lasting benefits in over 85% of cases. Early intervention and physical rehabilitation improve long-term outcomes.
Out-of-Pocket Costs
Medicare
CPT Code 63047 – Lumbar Laminectomy (Decompression): $271.76
CPT Code 63030 – Laminotomy (Partial Decompression): $225.06
CPT Code 22612 – Posterior Lumbar Fusion: $382.85
CPT Code 22630 – Interbody Fusion (PLIF/TLIF): $387.42
CPT Code 22842 – Instrumentation (Rods, Screws, Plates – 3–6 Segments): $185.26
Under Medicare, 80% of the approved cost for these surgical procedures is covered once the annual deductible is met. The patient is typically responsible for the remaining 20%. Supplemental insurance plans, such as Medigap, AARP, or Blue Cross Blue Shield, usually pay this 20% balance, which means patients often have no out-of-pocket costs for Medicare-approved spinal surgeries. These supplemental policies coordinate directly with Medicare to provide full coverage for procedures like decompression, fusion, and instrumentation.
If you have secondary insurance, such as an Employer-Based Plan, TRICARE, or Veterans Health Administration (VHA) coverage, it serves as a secondary payer after Medicare has processed the claim. Once your deductible is satisfied, these plans can cover the remaining coinsurance or balance. Deductibles for secondary policies generally range between $100 and $300, depending on your plan and whether the surgery is performed in-network.
Workers’ Compensation
If your lumbar canal stenosis developed as a result of a workplace injury or repetitive strain, Workers’ Compensation will pay for all surgical and hospital expenses related to decompression and fusion procedures. This includes the cost of implants, anesthesia, and postoperative care, leaving you with no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your lumbar stenosis was caused or worsened by a motor vehicle accident, No-Fault Insurance will fully cover all related diagnostic, surgical, and rehabilitation costs. The only potential out-of-pocket expense would be a small deductible based on your specific policy terms.
Example
George, a 68-year-old patient, underwent lumbar laminectomy (CPT 63047) and posterior interbody fusion (CPT 22630) to relieve severe back and leg pain caused by lumbar canal stenosis. His estimated Medicare out-of-pocket costs were $271.76 and $387.42. Because George had supplemental insurance through Medigap, the 20% that Medicare did not cover was paid in full, leaving him with no out-of-pocket expense for his surgery.
Frequently Asked Questions (FAQ)
Q. What causes lumbar canal stenosis?
A. The most common cause is age-related degeneration that leads to thickened ligaments, bone spurs, and disc bulging, narrowing the spinal canal.
Q. How is lumbar canal stenosis different from a herniated disc?
A. A herniated disc is a single-level problem caused by disc rupture, while stenosis often involves multiple levels with narrowing of the entire canal.
Q. Can exercise help with lumbar canal stenosis?
A. Yes. Stretching and core-strengthening exercises can relieve symptoms and improve posture. Physical therapy can also teach proper movement to reduce strain.
Q. When is surgery necessary?
A. Surgery is needed if pain persists beyond 6–12 weeks despite therapy or if you develop weakness, numbness, or bladder and bowel problems.
Summary and Takeaway
Lumbar canal stenosis is a common cause of lower back and leg pain due to narrowing of the spinal canal. Most patients improve with medications, physical therapy, and lifestyle changes. Surgery offers reliable relief for persistent or severe nerve compression. Early treatment, active rehabilitation, and healthy habits provide long-term improvement and restored mobility.
Clinical Insight & Recent Findings
A recent study compared bilateral laminoplasty with posterior lumbar interbody fusion (PLIF) for patients over 60 years old suffering from multi-level lumbar canal stenosis. Conducted over two years, the study evaluated 51 patients (26 laminoplasty, 25 PLIF) and found that bilateral laminoplasty achieved similar neurological and pain relief outcomes while offering several key advantages.
Laminoplasty resulted in significantly shorter operative times (1.8 vs. 3.2 hours), less blood loss (102 ml vs. 318 ml), and no transfusion requirements compared to PLIF, which had a 52% transfusion rate. Both groups experienced substantial improvements in pain and function, but the laminoplasty group reported better long-term disability scores on the Oswestry Disability Index.
The authors concluded that bilateral laminoplasty is a safe, motion-preserving alternative to fusion, particularly suitable for elderly patients with comorbidities such as hypertension and diabetes, offering effective decompression with reduced surgical trauma and faster recovery. (Study of bilateral laminoplasty versus PLIF for multi-level lumbar canal stenosis – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is performed by orthopedic spine surgeons or neurosurgeons, supported by anesthesiologists, rehabilitation specialists, and physical therapists.
When to See a Specialist?
You should see a spine specialist if you have:
- Persistent back or leg pain
- Difficulty walking long distances
- Tingling, numbness, or weakness in your legs
- Pain that improves when bending forward
When to Go to the Emergency Room?
Go to the ER immediately if you experience:
- Sudden loss of bladder or bowel control
- Severe leg weakness or numbness
- Inability to stand or walk
What Recovery Really Looks Like?
Most patients gradually resume normal activities within a few weeks. Walking tolerance improves, and pain subsides over time. Regular physical therapy enhances flexibility and prevents recurrence.
What Happens If You Ignore It?
Untreated lumbar stenosis can lead to chronic pain, progressive weakness, or permanent nerve damage. In severe cases, paralysis or loss of bladder control may occur.
How to Prevent It?
- Maintain good posture and spinal alignment.
- Engage in regular exercise, especially core strengthening.
- Avoid smoking and excess body weight.
- Practice safe lifting techniques to protect your back.
Nutrition and Bone or Joint Health
A diet rich in calcium, vitamin D, and protein supports spinal bone health. Stay hydrated and avoid processed foods that promote inflammation.
Activity and Lifestyle Modifications
Low-impact exercises such as walking, swimming, and yoga improve strength and flexibility. Take frequent breaks when standing or walking, and use ergonomic furniture for support.
Do you have more questions?
What exactly is lumbar canal stenosis?
Lumbar canal stenosis is a condition where the space in the spinal canal in the lower back becomes narrowed, which can compress the nerve roots and lead to various symptoms.
What causes lumbar canal stenosis?
The most common cause is degeneration due to aging. Other causes include traumatic injuries, congenital conditions, and changes in the spine such as herniated discs, arthritis, and bone spurs.
What are the symptoms of lumbar canal stenosis?
Symptoms include radicular pain (pain radiating down the legs), tingling, numbness, weakness, and neurogenic claudication (pain and heaviness in the legs when standing or walking).
How is lumbar canal stenosis diagnosed?
Diagnosis typically involves a physical examination and imaging studies, such as MRI or CT scans, to visualize the narrowing of the spinal canal and nerve root compression.
What conservative treatments are available?
Conservative treatments include pain relievers, anti-inflammatory medications, physical therapy exercises, and possibly cortisone injections.
Can lumbar canal stenosis improve without surgery?
Yes, many patients see improvement with conservative treatments such as medications, physical therapy, and lifestyle changes.
When should surgery be considered for lumbar canal stenosis?
Surgery is considered when symptoms persist despite conservative treatment, particularly if there is significant pain, weakness, or neurogenic claudication affecting quality of life.
What types of surgical procedures are available?
Common surgical procedures include decompression laminectomy, foraminotomy, and various fusion techniques (ALIF, LLIF, PLIF, TLIF).
What is the success rate of surgery for lumbar canal stenosis?
Surgery generally has a high success rate, with many patients experiencing significant relief from their symptoms.
What are the risks associated with lumbar spine surgery?
Risks include infection, bleeding, nerve damage, failure of the bones to fuse properly, and complications related to anesthesia.
What lifestyle changes can help manage lumbar canal stenosis?
Maintaining a healthy weight, staying active with appropriate exercises, and avoiding activities that exacerbate symptoms can help manage the condition.
Can lumbar canal stenosis recur after surgery?
While surgery can provide long-term relief, there is a possibility of recurrence, especially if the underlying degenerative processes continue.
Are there specific exercises that can help?
Yes, exercises that strengthen the core muscles of the back and improve flexibility can help stabilize the spine and reduce symptoms.
What is cauda equina syndrome and why is it serious?
Cauda equina syndrome is a severe condition where nerve compression leads to significant pain, weakness, and loss of bowel or bladder control. It requires immediate medical attention.
What is neurogenic claudication?
Neurogenic claudication is pain, heaviness, or weakness in the legs triggered by standing or walking, which is relieved by sitting or bending forward.
Can lumbar canal stenosis cause permanent nerve damage?
If left untreated, severe stenosis can lead to permanent nerve damage, but timely treatment can prevent this outcome.
How long is the recovery period after lumbar canal stenosis surgery?
Recovery time varies depending on the procedure and individual patient factors, but it typically ranges from a few weeks to a few months.
How can I prevent lumbar canal stenosis from worsening?
Staying active, maintaining a healthy weight, avoiding smoking, and following a regular exercise regimen can help prevent worsening of the condition.
Can physical therapy alone be effective in treating lumbar canal stenosis?
Physical therapy can be very effective for many patients, particularly those with mild to moderate symptoms.
Is lumbar canal stenosis a common condition?
Yes, it is a common condition, particularly among older adults due to the degenerative changes that occur with aging.
Can lumbar canal stenosis be detected early?
Early detection can occur through regular medical check-ups and imaging studies if symptoms are present.
What is the role of imaging studies in diagnosing lumbar canal stenosis?
Imaging studies, such as MRI and CT scans, are crucial for visualizing the extent of spinal canal narrowing and nerve compression.
Can lumbar canal stenosis affect both legs?
Yes, symptoms can affect one or both legs, depending on the severity and location of the stenosis.
Are there any dietary recommendations for managing lumbar canal stenosis?
While there are no specific dietary recommendations, maintaining a balanced diet to support overall health and a healthy weight can be beneficial.
What should I do if I experience sudden severe symptoms?
Seek immediate medical attention, especially if you experience sudden severe pain, weakness, or loss of bowel or bladder control, as these could indicate cauda equina syndrome.

