Adjacent Segment Disease (ASD) refers to new wear-and-tear changes that develop in the spinal segments above or below a previously fused area in the neck. These changes can occur years after a cervical fusion surgery and may lead to symptoms such as pain, stiffness, or nerve compression. While many cases can be managed without surgery, some patients eventually need another operation to stabilize the affected area.
How Common It Is and Who Gets It? (Epidemiology)
ASD is one of the more common long-term complications following cervical fusion. Studies show that about 25% of patients develop signs of adjacent segment degeneration within 10 years after surgery, though not all develop symptoms. It is more frequently seen in people under 60, women, and those with pre-existing degenerative changes or a history of smoking.
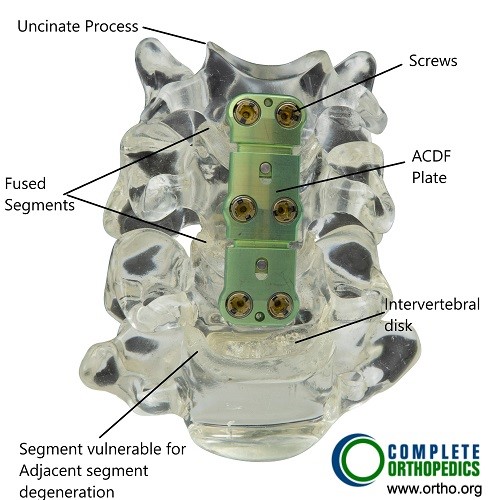
Bone model showing ACDF.
Why It Happens – Causes (Etiology and Pathophysiology)
When two or more neck bones are fused, the fused section no longer moves. To compensate, the segments just above and below move more than usual. This increased mechanical stress can gradually wear down the discs, joints, and ligaments of those nearby levels.
Other contributing factors include:
- Pre-existing disc degeneration before the first surgery
- Surgical technique, especially if motion is overly restricted
- Patient factors, such as age, activity level, and bone quality
Over time, these stresses can lead to disc herniation, loss of disc height, bone spurs, or narrowing of the spinal canal.
How the Body Part Normally Works? (Relevant Anatomy)
The cervical spine is made of seven vertebrae separated by intervertebral discs that act as cushions. Each segment moves slightly to allow overall neck motion. Facet joints in the back of the spine help guide movement, while ligaments and muscles provide stability.
When one level is fused, motion stops at that point. The adjacent discs and joints take on extra strain, which can accelerate aging or injury in those areas.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of ASD are often similar to the problems that led to the original surgery. Common signs include:
- Persistent or worsening neck pain
- Pain radiating to the shoulders, arms, or upper back
- Stiffness or reduced neck motion
- Numbness, tingling, or weakness in the arms or hands
- Headaches starting at the base of the skull and radiating forward
Severe cases can cause spinal cord compression (myelopathy), leading to clumsiness, balance problems, or changes in bladder control.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis begins with a full medical history and physical exam. Your doctor checks muscle strength, reflexes, and sensation in the arms and legs, and observes walking and balance.
Imaging tests may include:
- X-rays to see alignment and hardware position
- CT scans for detailed views of bone healing and possible overgrowth
- MRI to assess soft tissues and nerve compression
These studies help distinguish ASD from infection, pseudoarthrosis (non-healing fusion), or degeneration at unrelated spinal levels.
Classification
Doctors often describe ASD in two ways:
- Adjacent Segment Degeneration (ASDeg): Imaging shows wear and tear but without symptoms.
- Adjacent Segment Disease (ASDis): Imaging changes plus pain, numbness, or weakness.
The severity is then graded based on the amount of disc space collapse, bone spur formation, or nerve compression seen on scans.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may mimic ASD include:
- Disc herniation at a non-adjacent level
- Cervical spondylosis (age-related arthritis)
- Muscle strain or facet joint pain
- Infection or failed fusion at the original site
Treatment Options
Non-Surgical Care
Most cases begin with conservative treatment:
- Medications: Anti-inflammatory drugs, pain relievers, or muscle relaxants.
- Physical therapy: Strengthening neck and shoulder muscles to improve support and flexibility.
- Lifestyle changes: Avoiding prolonged sitting, adjusting posture, quitting smoking, and maintaining a healthy weight.
- Injections: Corticosteroid injections may reduce inflammation and pain temporarily.
Surgical Care
Surgery is considered when non-surgical care fails or if nerve compression causes weakness or coordination problems.
Options include:
- Extension of fusion: Adding the next affected level to the existing fusion to stabilize the spine.
- Cervical disc replacement: In select patients, an artificial disc can restore motion and potentially reduce future stress on other segments.
Your surgeon selects the best approach based on symptoms, alignment, and overall spinal health.
Recovery and What to Expect After Treatment
Recovery depends on the type of treatment.
- Non-surgical care can relieve symptoms within weeks to months with consistent therapy.
- Surgery typically requires a short hospital stay followed by light activity for several weeks. Full recovery and bone healing after fusion may take several months.
Physical therapy after surgery helps restore mobility and reduce stiffness.
Possible Risks or Side Effects (Complications)
Potential risks include infection, nerve injury, bleeding, or hardware failure. After fusion, the risk of further adjacent-level degeneration persists, but newer techniques aim to reduce this chance.
Long-Term Outlook (Prognosis)
Most patients achieve good pain relief and improved function. Proper rehabilitation and attention to posture and ergonomics can slow or prevent future degeneration. Continued follow-up is important to monitor for changes in nearby spinal segments.
Out-of-Pocket Costs
Medicare
CPT Code 22010 – Sequestrectomy (Debridement): $238.90
CPT Code 22600 – Spinal Fusion (C1–C2): $322.92
CPT Code 22843 – Occipitocervical Fusion: $198.65
CPT Code 63300 – Lesion Decompression or Biopsy (Upper Cervical Spine): $450.25
Under Medicare, patients are responsible for 20% of the approved amount for these spine procedures once the annual deductible has been met. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—typically pay the remaining 20%, leaving patients with little or no out-of-pocket cost for Medicare-approved services. These plans work together with Medicare to close the coverage gap, especially for complex spine surgeries requiring fusion or decompression at the upper cervical levels.
If you have secondary insurance, such as an Employer-Based Plan, TRICARE, or Veterans Health Administration (VHA) coverage, it functions as a secondary payer after Medicare. Once your Medicare deductible is met, these secondary plans often cover the remaining balance, including co-insurance or other costs. Secondary plans may have their own deductibles, generally ranging from $100 to $300 depending on the policy and network of the treating facility.
Workers’ Compensation
If your upper cervical spine condition or injury is related to a work accident, Workers’ Compensation will fully cover the cost of all procedures, including debridement, fusion, or decompression. This coverage also includes hospitalization, postoperative rehabilitation, and necessary imaging, leaving you with no out-of-pocket expenses.
No-Fault Insurance
If your upper cervical spine injury was caused by a motor vehicle accident, No-Fault Insurance will cover all medical and surgical costs for evaluation and treatment, including fusion or decompression procedures. You may only be responsible for a small deductible depending on your insurance policy terms.
Example
James, a 60-year-old patient, required a C1–C2 fusion (CPT 22600) and occipitocervical fusion (CPT 22843) following a traumatic instability at the upper cervical junction. His Medicare out-of-pocket cost would have been $322.92 and $198.65, respectively. Because he had supplemental insurance through Blue Cross Blue Shield, the remaining 20% not covered by Medicare was fully paid, resulting in no out-of-pocket expense for his surgery.
Frequently Asked Questions (FAQ)
Q. Is ASD inevitable after fusion?
A. No. Not every patient develops it. Risk depends on age, spinal mechanics, and lifestyle.
Q. Can physical therapy help?
A. Yes. Targeted therapy can strengthen support muscles and ease pain.
Q. Will another fusion always be required?
A. Only if symptoms persist or neurological deficits appear. Many patients manage well without further surgery.
Summary and Takeaway
Adjacent Segment Disease is a long-term effect that can occur after cervical fusion due to extra stress on nearby spinal levels. While many patients improve with medication and therapy, some may eventually require additional surgery. With proper rehabilitation, healthy habits, and ongoing medical follow-up, most people maintain a good quality of life and lasting relief from neck pain.
Clinical Insight & Recent Findings
A recent review analyzed risk factors and treatment strategies for Adjacent Segment Disease (ASD), a common complication following cervical fusion. The study highlighted that altered spinal biomechanics after fusion—where stress shifts to levels above or below the fused segment—accelerates disc degeneration and facet joint arthritis.
Patient factors such as age, obesity, osteoporosis, diabetes, and pre-existing degeneration increase susceptibility, while surgical variables like fusion length, alignment, and soft-tissue disruption further elevate risk. Early management typically includes rehabilitation, anti-inflammatory medications, and epidural or facet joint injections to control pain and preserve mobility. For persistent neurological symptoms or instability, motion-preserving techniques such as total disc replacement and minimally invasive approaches like oblique lateral interbody fusion (OLIF) show favorable outcomes.
Emerging regenerative treatments—stem cell therapy, exosome-based repair, and 3D-printed interbody cages—are under investigation for restoring disc biomechanics and preventing further degeneration. (Study of risk factors and treatment strategies for adjacent segment disease following cervical fusion – See PubMed.)
Who Performs This Treatment? (Specialists and Team Involved)
Treatment is led by orthopedic spine surgeons and neurosurgeons, supported by physical therapists, radiologists, and pain management specialists.
When to See a Specialist?
Consult a spine specialist if you have:
- New or worsening neck or arm pain after prior fusion
- Tingling, numbness, or weakness in your arms or hands
- Reduced neck movement or stiffness
When to Go to the Emergency Room?
Seek immediate medical attention if you develop:
- Sudden arm or leg weakness
- Loss of coordination or bladder control
- Severe neck pain after an injury or fall
What Recovery Really Looks Like?
Recovery varies, but most patients regain comfort and function through a combination of therapy and lifestyle changes. After surgery, gradual activity resumption and physical therapy lead to long-term improvement.
What Happens If You Ignore It?
Untreated ASD can lead to worsening pain, nerve compression, and spinal cord problems that may eventually require urgent surgery. Early evaluation prevents complications and maintains neck function.
How to Prevent It?
- Maintain good posture and neck alignment
- Stay active with safe stretching and strengthening exercises
- Avoid smoking and excessive strain on the neck
- Follow up regularly after fusion surgery to monitor nearby segments
Nutrition and Bone or Joint Health
Strong bones require a diet rich in calcium, vitamin D, and protein. Staying hydrated and maintaining a healthy weight reduce pressure on the spine and joints.
Activity and Lifestyle Modifications
Engage in low-impact exercises such as swimming, walking, or yoga. Use ergonomic work setups and avoid sudden twisting or heavy lifting. Regular movement keeps the spine flexible and balanced.
Do you have more questions?
What is the typical timeline for the development of ASD after cervical fusion?
Typically, ASD can manifest anywhere from 2 to 10 years post-surgery. However, it’s crucial to understand that this timeline can vary significantly based on individual factors such as the patient’s age, the extent of the initial surgery, and their overall spinal health.
Are there specific types of cervical fusion that are more likely to result in ASD?
Yes, multi-level fusions are more prone to leading to ASD compared to single-level fusions. This is because more segments are immobilized, increasing the biomechanical stress on the adjacent unfused segments.
What are the risks of not treating ASD if symptoms are mild?
Mild symptoms can gradually worsen if left untreated, potentially leading to more severe pain, loss of function, and neurological deficits. Early intervention can help manage symptoms more effectively and prevent progression.
How is the decision made between non-surgical and surgical treatment for ASD?
The decision is based on the severity and progression of symptoms, the degree of degeneration observed in imaging studies, and the patient’s overall health and lifestyle. Typically, we start with conservative treatments and consider surgery if those measures fail to provide adequate relief.
Are there any lifestyle changes that can help manage ASD symptoms?
Absolutely. Maintaining a healthy weight, avoiding heavy lifting and high-impact activities, practicing good posture, and quitting smoking are all beneficial. Additionally, ergonomic adjustments at work and home can help reduce stress on the spine.
How effective are pain medications in managing ASD?
Pain medications, including NSAIDs and muscle relaxants, can be effective in managing pain and inflammation but should be part of a broader treatment strategy that includes physical therapy and lifestyle modifications.
Is it safe to engage in physical activities and sports after cervical fusion surgery?
Low-impact activities such as swimming, walking, and cycling are generally safe and encouraged. However, high-impact sports and activities that put significant strain on the neck should be avoided. Always consult your surgeon before resuming any physical activity.
What role do ergonomic adjustments play in managing ASD?
Ergonomic adjustments are crucial. Proper workstation setup, supportive chairs, and correct posture during daily activities can significantly reduce the mechanical stress on the cervical spine, helping to manage ASD symptoms.
Can chiropractic care help with ASD?
While some patients find relief from chiropractic care, it is essential to approach this cautiously. Manipulations should be gentle, and it is crucial to consult with your surgeon before undergoing chiropractic treatment to ensure it’s safe for your specific condition.
How often should follow-up appointments be scheduled after cervical fusion surgery?
Follow-up appointments should be scheduled immediately post-surgery, at six weeks, three months, six months, and annually thereafter, or more frequently if there are symptoms suggestive of ASD.
Can ASD be detected early through regular imaging?
Yes, regular imaging such as X-rays, MRIs, or CT scans can help detect early degenerative changes in adjacent segments, allowing for earlier intervention and better management of the condition.
Are there any genetic factors that increase the risk of developing ASD?
While there is no specific genetic marker for ASD, individuals with a family history of degenerative disc disease or other spinal conditions may be at a higher risk.
How does the recovery process from ASD surgery compare to the initial cervical fusion surgery?
The recovery process for ASD surgery is generally similar to the initial surgery, involving a period of immobilization followed by rehabilitation. However, the specifics can vary based on the extent of the surgery and the patient’s overall health.
What are the potential complications of surgery for ASD?
Potential complications include infection, blood loss, nerve damage, and the risk of further degeneration at other adjacent segments. Nonunion or improper healing of the fusion site is also a concern.
Can wearing a cervical collar help in managing ASD?
Wearing a cervical collar can provide short-term relief by stabilizing the neck and reducing movement. However, long-term use is not recommended as it can lead to muscle atrophy and decreased neck strength.
Are there any new advancements in technology or techniques that might reduce the risk of ASD?
Yes, advancements such as artificial disc replacement and motion-preserving surgical techniques aim to maintain more natural movement in the spine, potentially reducing the stress on adjacent segments and lowering the risk of ASD.
How does age affect the risk and progression of ASD?
Older age is associated with increased risk due to the natural degenerative processes of the spine. Older patients often have pre-existing degenerative changes, which can accelerate the development and progression of ASD.
What kind of support systems are beneficial for patients dealing with ASD?
Support systems including physical therapy, patient education programs, counseling, and support groups can help patients manage symptoms and improve their quality of life. A multidisciplinary approach often yields the best outcomes.
Can nutritional supplements help in the management of ASD?
Nutritional supplements like glucosamine and chondroitin may support joint health, although evidence of their efficacy varies. Omega-3 fatty acids may help reduce inflammation. Always consult with your doctor before starting any supplements.
How does obesity impact ASD?
Obesity increases the mechanical load on the spine, which can accelerate degeneration and worsen ASD symptoms. Weight management through diet and exercise is an important aspect of treatment.
What is the role of alternative therapies like acupuncture in managing ASD?
Acupuncture can provide pain relief for some individuals and may be a useful adjunct to conventional treatments. It’s important to discuss this with your healthcare provider to ensure it’s safe and appropriate for your condition.
Can psychological factors impact the experience of ASD symptoms?
Yes, psychological factors such as stress, anxiety, and depression can exacerbate the perception of pain and impact overall health. Addressing these factors through counseling and stress management techniques is important.
How can patients prepare for potential future ASD when planning their initial cervical fusion surgery?
Patients should discuss the potential for ASD with their surgeon and consider surgical options that minimize stress on adjacent segments. Engaging in pre-surgical physical therapy and adopting a healthy lifestyle can also help.
What are the long-term outlooks for patients who develop ASD after cervical fusion?
The long-term outlook varies but can be positive with appropriate management. Many patients manage symptoms effectively with conservative treatments, and surgical intervention can restore function and alleviate pain when necessary. Regular follow-ups and a proactive approach to spine health are key.

