Posterior cervical fusion combined with laminectomy is a surgical approach often used to treat cervical spine conditions that involve multi-level compression of the spinal cord or nerve roots. This procedure is aimed at stabilizing the cervical spine after decompression surgery to prevent further neurological deterioration. It is typically recommended for patients with cervical spondylotic myelopathy (CSM) or those experiencing significant pain, weakness, or neurological deficits due to spinal cord compression.
How Common It Is and Who Gets It? (Epidemiology)
Cervical spondylotic myelopathy (CSM) is the most common indication for posterior cervical fusion with laminectomy. It is generally seen in individuals over the age of 50, as age-related degenerative changes, such as arthritis or disc degeneration, lead to narrowing of the spinal canal. Patients with multi-level spinal cord compression or those with congenital spinal canal stenosis may also be candidates for this surgery.
Why It Happens – Causes (Etiology and Pathophysiology)
The need for posterior cervical fusion and laminectomy arises when the spinal cord or nerve roots in the cervical spine are compressed due to degenerative changes, disc herniation, or bone spurs. This compression can result in symptoms like neck pain, numbness, weakness in the arms or legs, loss of balance, and, in severe cases, loss of bowel or bladder function. Laminectomy is performed to remove the pressure from the spinal cord, while fusion is done to stabilize the spine, which becomes unstable after removing bone structures.
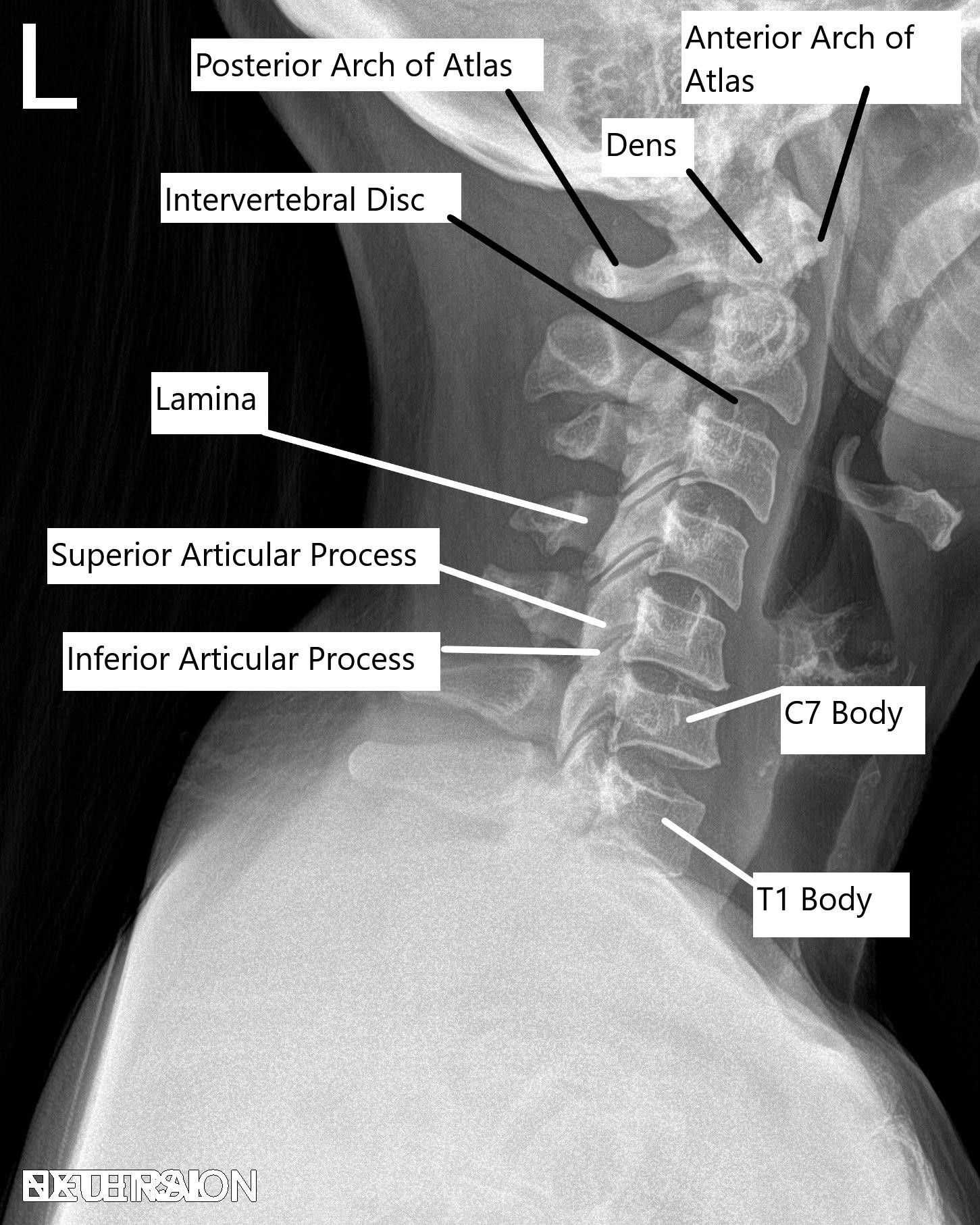
Cervical Spine X-ray in Lateral view.
How the Body Part Normally Works? (Relevant Anatomy)
The cervical spine is composed of seven vertebrae (C1 to C7), which are separated by intervertebral discs. The vertebrae protect the spinal cord and allow for movement in the neck. The foramen, or small openings between the vertebrae, allow spinal nerves to exit the spinal cord and travel to different parts of the body. When these structures become compromised due to degenerative changes, compression can occur, leading to pain and other neurological symptoms.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of cervical spondylotic myelopathy and other conditions treated by posterior cervical fusion and laminectomy include:
- Chronic Neck Pain: Often accompanied by radiating pain into the shoulders, arms, and hands.
- Numbness or Tingling: Sensory changes in the arms or hands.
- Weakness: Difficulty lifting objects or performing daily activities due to muscle weakness.
- Balance Issues: Difficulty walking or maintaining balance.
- Loss of Bowel/Bladder Control: In severe cases, compression of the spinal cord can lead to incontinence.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis is typically made through a combination of clinical evaluation and imaging studies, including:
- X-rays: To assess the alignment of the cervical spine.
- MRI: Provides detailed images of soft tissues, including the spinal cord and discs.
- CT Scans: Helpful for assessing bone spurs and identifying areas of compression.
- Neurological Evaluation: To assess the extent of motor or sensory deficits.
Classification
Cervical spine fusion surgeries are typically classified by the approach:
- Posterior Cervical Fusion and Laminectomy: Performed from the back of the neck, often involving multi-level decompression and fusion.
- Anterior Cervical Discectomy and Fusion (ACDF): A similar procedure done from the front of the neck, typically for single or two-level disc herniations.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions like cervical herniated discs, cervical radiculopathy, or thoracic outlet syndrome can cause similar symptoms, including neck pain, radiating pain, and weakness. Proper imaging and clinical evaluation are essential to differentiate these conditions from those requiring posterior cervical fusion and laminectomy.
Treatment Options
Non-Surgical Care: Physical therapy, anti-inflammatory medications, and epidural steroid injections are often used to manage symptoms of cervical spine compression.
Surgical Care: Posterior cervical fusion with laminectomy is typically performed when conservative treatments fail or when significant neurological deficits are present. This surgery involves decompression of the spinal cord followed by stabilization with screws, rods, and bone grafts.
Recovery and What to Expect After Treatment
- Hospital Stay: Patients typically stay in the hospital for a few days to manage pain and monitor for complications.
- Pain Management: Pain medications will be prescribed to manage post-surgical discomfort.
- Physical Therapy: Rehabilitation exercises will help restore neck strength and mobility.
- Activity Restrictions: Patients will be advised to avoid heavy lifting and strenuous activities during the initial recovery phase, with a gradual return to normal activities.
Recovery from posterior cervical fusion and laminectomy can take several months, and the improvement in neurological function may continue over time, although complete recovery is not always guaranteed.
Possible Risks or Side Effects (Complications)
As with any surgery, there are risks involved with posterior cervical fusion and laminectomy, including:
- Infection: Risk of infection at the surgical site, particularly in surgeries performed from the back of the neck.
- Nerve Injury: Injury to the spinal cord or nerve roots, potentially leading to new or worsened neurological symptoms.
- Implant Failure: The screws or rods used to stabilize the spine may shift or break, requiring further intervention.
- Cerebrospinal Fluid (CSF) Leak: A rare complication that may require additional surgery.
- Adjacent Segment Degeneration: Additional stress on the segments of the spine adjacent to the fused area may lead to further degeneration.
Long-Term Outlook (Prognosis)
The long-term outlook for patients undergoing posterior cervical fusion and laminectomy is generally positive, especially for those with cervical spondylotic myelopathy and multi-level compression. The surgery effectively stabilizes the spine and relieves pressure on the spinal cord, leading to improved pain relief and neurological function. However, full recovery can take several months, and in some cases, neurological recovery may not be complete.
Out-of-Pocket Cost
Medicare
CPT Code 22600 – Posterior Cervical Fusion: $322.92
Under Medicare, 80% of the approved cost for this procedure is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—usually cover this 20%, leaving most patients with little to no out-of-pocket expenses for Medicare-approved posterior cervical fusion surgery. These supplemental plans work directly with Medicare to ensure full coverage for complex cervical spine surgeries.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare has processed your claim. After your deductible is satisfied, the secondary plan may cover any remaining balance, including coinsurance or small residual charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on the policy and provider network.
Workers’ Compensation
If your cervical spine condition requiring fusion is related to a work injury, Workers’ Compensation will cover the entire cost of the procedure, including hospitalization, instrumentation, and rehabilitation. You will have no out-of-pocket costs under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your cervical spine injury is the result of a motor vehicle accident, No-Fault Insurance will cover all medical and surgical costs associated with posterior cervical fusion. The only potential out-of-pocket cost may be a small deductible depending on your specific insurance policy terms.
Example
Tom, a 62-year-old patient with cervical instability and nerve compression, underwent posterior cervical fusion (CPT 22600). His Medicare out-of-pocket cost was $322.92. Since he had supplemental insurance through AARP Medigap, the 20% that Medicare did not cover was fully paid, leaving him with no out-of-pocket expenses for his surgery.
Frequently Asked Questions (FAQ)
Q. How long does recovery take after posterior cervical fusion surgery?
A. Most patients can return to normal activities within 6 to 12 weeks, although full recovery may take several months.
Q. What are the advantages of posterior cervical fusion over anterior cervical fusion?
A. Posterior fusion is often used when there is multi-level compression or when anterior approaches are not feasible. It provides a broader approach for decompression and can be used for more complex cases.
Summary and Takeaway
Posterior cervical fusion and laminectomy is a vital surgical procedure for treating conditions like cervical spondylotic myelopathy, which involves multi-level compression of the spinal cord. While the surgery carries risks, it offers significant relief from pain and neurological symptoms in appropriately selected patients. With proper surgical technique and post-operative care, most patients experience significant improvement in their condition.
Clinical Insight & Recent Findings
A recent study analyzed the outcomes of posterior cervical fusion (PCF) surgeries performed between 2012 and 2022, with a focus on an aging patient population and increasing medical complexity.
The findings highlighted that despite an increase in comorbidities such as diabetes, hypertension, and heart failure, the complication rates, including infection and reoperation, remained relatively stable. Additionally, the study showed a significant reduction in blood transfusion requirements and a slight decrease in the average length of stay.
The results emphasize that PCF continues to be an effective surgical option for managing cervical spondylotic myelopathy, even in older, medically complex patients. (“Study of clinical outcomes of posterior cervical fusion – See PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Orthopedic spine surgeons or neurosurgeons specializing in cervical spine disorders typically perform posterior cervical fusion and laminectomy. The surgical team may also include anesthesiologists, nurses, and rehabilitation specialists to ensure optimal recovery.
When to See a Specialist?
If you experience persistent neck pain, numbness, weakness, or difficulty with balance, or if you’ve been diagnosed with a cervical spine condition, it’s important to consult a specialist for a comprehensive evaluation.
When to Go to the Emergency Room?
Seek immediate care if you experience sudden weakness, difficulty breathing, or loss of bowel or bladder control, as these may be signs of a spinal emergency.
What Recovery Really Looks Like?
Recovery typically involves a gradual improvement in symptoms, with patients returning to normal activities within a few weeks to months. Full recovery can take longer, and physical therapy is essential for restoring strength and mobility.
What Happens If You Ignore It?
Ignoring cervical spine issues can lead to permanent nerve damage, paralysis, or further disability. Early surgical intervention can help prevent these outcomes and improve long-term function.
How to Prevent It?
Maintaining good posture, avoiding excessive strain on the neck, and performing regular neck-strengthening exercises can help prevent cervical spine problems. Regular check-ups with a healthcare provider can also help catch issues early before they require surgery.
Nutrition and Bone or Joint Health
Adequate intake of calcium and vitamin D is essential for maintaining healthy bones, which support the cervical spine. Proper nutrition helps prevent degenerative changes and promotes healing after surgery.
Activity and Lifestyle Modifications
After surgery, patients should focus on gentle rehabilitation exercises to restore mobility and strength in the neck. Avoiding heavy lifting and high-impact activities is essential for a successful recovery.
Do you have more questions?
How do I prepare for posterior cervical fusion surgery?
Preparation includes medical evaluations, discontinuing certain medications, arranging post-surgery care, and following specific preoperative instructions from your healthcare team.
What are the alternative treatments to posterior cervical fusion?
Alternatives include physical therapy, medications, steroid injections, and other surgeries like anterior cervical discectomy and fusion (ACDF).
What are the risks of not undergoing the surgery?
Risks include worsening symptoms, increased pain, potential permanent nerve damage, and loss of function.
How long does the posterior cervical fusion surgery take?
The procedure typically lasts 2-4 hours, depending on the complexity and the number of levels being fused.
What are bone grafts, and where do they come from?
Bone grafts are materials promoting bone fusion, sourced from your body (autograft), a donor (allograft), or synthetic alternatives.
Will I have scars after the surgery?
Yes, there will be a scar at the incision site on the back of your neck. Its size and visibility depend on the surgical approach used.
How long will I need to stay in the hospital after surgery?
Most patients stay in the hospital for 2-3 days post-surgery for monitoring and initial recovery.
What should I expect in terms of pain after surgery?
Post-operative pain is common but manageable with medications, typically subsiding significantly within a few weeks.
When can I resume normal activities after the surgery?
Light activities can resume within a few weeks, but strenuous activities should be avoided for 3-6 months.
How will I know if the fusion was successful?
Success is assessed through follow-up appointments, imaging tests, and the resolution of pre-surgery symptoms.
Can the hardware used in the fusion cause problems later?
Rarely, hardware complications such as loosening or breakage can occur, potentially requiring additional surgery.
Will I lose any range of motion in my neck after the surgery?
Some loss of range of motion is expected, especially with multi-level fusions, but most patients adapt well.
Are there long-term restrictions after the surgery?
Long-term restrictions might include avoiding high-impact activities that strain the neck.
What is the success rate of posterior cervical fusion?
Success rates are high, with significant pain relief and improved function reported in over 80-90% of cases.
Can I still experience neck pain after the surgery?
Some patients may experience mild residual neck pain, but it is generally much less severe than before surgery.
What are the most common complications of this surgery?
Common complications include infection, nerve damage, non-union of the vertebrae, and hardware issues.
What are the signs of a post-surgery infection?
Signs of infection include redness, swelling, increased pain at the incision site, drainage or pus, fever, and chills.
How is a non-union treated if the bones don’t fuse properly?
Non-union may require additional surgical intervention to re-stabilize the spine, possibly involving new bone grafts or revised hardware placement.
What can I do to minimize the risk of complications?
To minimize risks, follow all post-operative care instructions, avoid smoking, maintain a healthy diet, and attend all scheduled follow-up appointments.
How often will I need to follow up with my surgeon after the surgery?
Follow-up appointments are typically scheduled at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year post-surgery to monitor progress and address any issues.

