Hip fracture after total hip replacement may involve a fracture of the bone around the implant or of the bone directly surrounding the implant. Periprosthetic fractures are increasing in incidence as more and more people are getting hip replacement surgeries.
The higher physical demand of the elderly patient may also play a role in the increased incidence of periprosthetic fractures. The management of fractures after hip replacement is often surgical and may require the use of complex instruments or implants.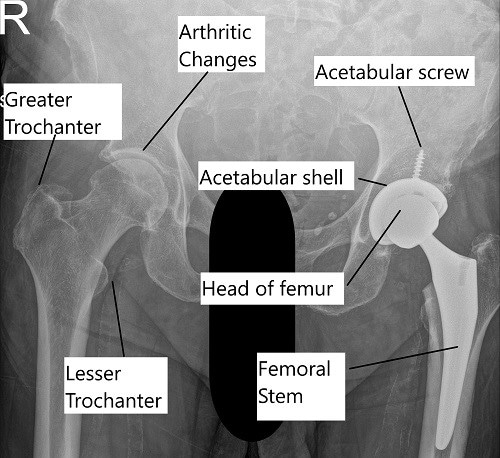
X-ray showing a total hip replacement surgery.
The majority of the periprosthetic fractures occur years after the surgery due to loosening of the implanted secondary to wear and tear or aseptic loosening. However, fractures may also occur during the surgery, especially in patients with metabolic bone disease such as osteoporosis.
Intraoperative acetabulum fractures
Intraoperative fractures occur during the surgery. Cementless fixation, not removing enough bone (under-reaming) before the impaction, metabolic bone disease such as osteoporosis, mal-formation of the acetabulum socket, any history of prior radiation therapy are all risk factors for intraoperative acetabulum fractures.
The fractures are evaluated intraoperative and if found to be stable, only observation is done along with protected weight-bearing. In case the fracture is found to be unstable, an acetabular component revision is done which may involve the use of jumbo cups or additional screws. In cases, where there is bone loss or extensive fracture, additional fixation may be necessary for the form of plates and screws along with bone graft.
Intraoperative femur fractures
Intraoperative femur fractures occur more often during revision total hip replacement rather than primary hip replacement. The fractures occur often during bone preparation of the femur for implant insertion. May occur as a result of a wrong technique, implants or instrument mismatch, or use of excessive force.
Patients with underlying bone metabolic disorders such as osteoporosis are also at an increased risk of intraoperative fractures. The management depends upon the level of fracture and the extent of the fracture. Usually, cables, wires, plates may be used to fix the fracture which is followed by re-insertion of the same implant or an implant with a longer stem.
Postoperative femur fractures
The fractures around the prosthetic joint occurring after the surgery are known as postoperative fractures. The postoperative fracture may occur in the early postoperative period or may occur years after the initial surgery.
Cementless hip arthroplasties are prone to fracture in the first 6 months of the surgery. Similar to intraoperative fractures, patients with diseases such as osteoporosis are at an increased risk of fracture. Compared to cementless fixation, cemented hip arthroplasties often fracture years after the surgery.
The postoperative fracture in the early postoperative period occurs as a result of stressors arising in the area of bone preparation for the implants. The fracture may be located near the upper part of the prosthesis. Cemented hip replacement often fractures below the lower end of the prosthesis.
The periprosthetic fractures occurring years after the initial surgery often occur as a result of aseptic loosening, or due to increased activity level of the patient.
The management of postoperative femur periprosthetic fracture depends upon the type and the extent of the fracture. Fractures of the greater and the lesser trochanter may be managed with the nonoperative treatment in the form of protected weight-bearing.
Displaced fractures may require the use of plates, wires, and screws. The implants may need to be revised along with fixation with other implants. The revised implants may have a longer stem or may be modified to accommodate the screws and plates.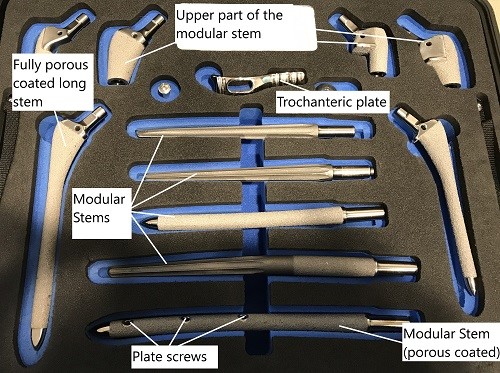
Various revision hip replacement implants.
Summary
The periprosthetic fractures after hip replacement often result in severe pain, disability, inability to bear weight, unequal leg length, or abnormal position of the leg. The symptoms are usually serious enough to warrant a visit to the ER and the patients are admitted to the hospital. Often patients may have multiple comorbid diseases that may require stabilization before the patients are fit for surgery.
The management largely depends upon the type and extent of the fracture and is usually surgical. The rehabilitation period following a periprosthetic fracture is usually longer compared to primary surgery. The patients may need to stay in the hospital longer. Rehabilitation usually involves therapy and pain management.
There may be potential complications of deep vein thrombosis, infection, blood loss, nerve injury, re-fracture, non-union of the fracture, leg length discrepancy, etc. Hip replacement surgeries are highly successful surgeries and the incidence of fracture is very low. Speak with your orthopedic surgeon regarding the risk of fracture and the management of periprosthetic fractures.
Research Spotlight
A recent study aimed to predict periprosthetic femoral fractures (PFF) after total hip arthroplasty (THA) by constructing a nomogram model. This model incorporated six key risk factors: age, sex, hip revision, non-cemented prosthesis, trauma history, and osteoporosis.
The study involved 2,528 patients and used logistic regression analysis to identify high-risk populations. The nomogram showed strong predictive accuracy across multiple cohorts and has been externally validated.
The findings emphasize the importance of individualized risk assessments and proactive management strategies for patients undergoing THA to reduce the risk of PFF. (“Study on predicting hip fractures after total hip replacement surgery – see PubMed.“)
Do you have more questions?
What are the symptoms of a periprosthetic fracture, and how can I differentiate them from normal post-surgery discomfort?
Periprosthetic fracture symptoms may include severe pain, disability, difficulty bearing weight, leg length discrepancy, or abnormal leg positioning. Differentiating these from normal post-surgery discomfort can be challenging, but any significant change in symptoms should be promptly reported to your healthcare provider.
Are there any specific risk factors that increase the likelihood of experiencing a periprosthetic fracture after hip replacement surgery?
Risk factors for periprosthetic fractures may include underlying bone metabolic disorders such as osteoporosis, previous radiation therapy, implant-related factors, or excessive force during surgery. Your surgeon can assess your individual risk profile and provide personalized recommendations.
What steps can I take to minimize my risk of experiencing a periprosthetic fracture, both during and after surgery?
If I experience a periprosthetic fracture, what immediate actions should I take, and when should I seek medical attention?
In the event of a suspected periprosthetic fracture, it’s crucial to seek medical attention promptly. Follow any instructions provided by your surgeon or healthcare provider, and avoid weight-bearing or movement that exacerbates symptoms until evaluated.
If I experience a periprosthetic fracture, what immediate actions should I take, and when should I seek medical attention?
In the event of a suspected periprosthetic fracture, it’s crucial to seek medical attention promptly. Follow any instructions provided by your surgeon or healthcare provider, and avoid weight-bearing or movement that exacerbates symptoms until evaluated.
What diagnostic tests are typically performed to confirm a periprosthetic fracture, and how accurate are these tests in detecting fractures?
Diagnostic tests such as X-rays, CT scans, or MRI scans may be used to confirm a periprosthetic fracture. These tests are generally accurate in detecting fractures, but your healthcare provider may recommend additional imaging or tests based on clinical suspicion.
What are the different types of periprosthetic fractures, and how does the type of fracture impact treatment decisions?
Periprosthetic fractures can vary in location, severity, and stability, which influences treatment decisions. Understanding the specific type of fracture and its implications allows your healthcare team to develop an appropriate treatment plan tailored to your needs.
What are the potential complications associated with periprosthetic fractures, and how are these complications managed?
Complications of periprosthetic fractures may include infection, blood loss, nerve injury, non-union, or leg length discrepancy. Treatment strategies aim to address these complications promptly through surgical intervention, rehabilitation, and ongoing monitoring.
What is the typical recovery timeline following surgical treatment for a periprosthetic fracture, and what can I expect during the rehabilitation process?
Recovery from a periprosthetic fracture surgery varies depending on the fracture severity and individual factors. Rehabilitation typically involves physical therapy, pain management, and gradual return to activities under the guidance of your healthcare team.
Are there any lifestyle modifications or precautions I should implement to reduce the risk of experiencing a periprosthetic fracture in the future?
Lifestyle modifications such as maintaining a healthy weight, avoiding excessive force or trauma to the hip, and adhering to prescribed activity guidelines can help minimize the risk of future fractures. Your surgeon can provide personalized recommendations based on your circumstances.
What support resources are available to assist patients and their families in coping with the physical and emotional challenges associated with periprosthetic fractures?
Support resources such as patient education materials, support groups, or counseling services may be beneficial for individuals navigating the challenges of periprosthetic fractures. Your healthcare provider can connect you with relevant resources and support networks.
Is there a specific follow-up schedule or monitoring plan after experiencing a periprosthetic fracture, and how often should I expect to see my healthcare provider?
Your healthcare provider will establish a follow-up schedule based on your individual needs and the nature of your fracture. Regular appointments may be necessary to monitor healing progress, address any concerns, and adjust treatment as needed.
Are there any dietary recommendations or supplements that can support bone health and reduce the risk of periprosthetic fractures?
Maintaining a balanced diet rich in calcium, vitamin D, and other nutrients essential for bone health may help support fracture healing and reduce the risk of future fractures. Your healthcare provider can provide dietary recommendations or recommend supplements if needed.
How does the risk of periprosthetic fractures differ between different types of hip replacement implants, and are there implant options that may lower this risk?
The risk of periprosthetic fractures may vary depending on the type of hip replacement implant used. Some implants may be associated with a higher risk of fractures than others. Your surgeon can discuss implant options and their associated risks to help you make informed decisions.
What are the long-term implications of experiencing a periprosthetic fracture, and how might it affect the longevity and function of my hip replacement?
Periprosthetic fractures can have long-term implications on the function and longevity of your hip replacement. Understanding these implications allows you and your healthcare team to develop appropriate management strategies and optimize outcomes.
Are there any alternative treatment options or technologies available for managing periprosthetic fractures that I should be aware of?
Emerging technologies and treatment modalities may offer alternative approaches to managing periprosthetic fractures. Your healthcare provider can discuss any innovative treatments or procedures that may be suitable for your specific situation.
How can I ensure proper home safety and fall prevention measures to reduce the risk of experiencing a periprosthetic fracture at home?
Implementing home safety measures such as removing tripping hazards, installing grab bars, and using assistive devices can help reduce the risk of falls and subsequent fractures. Your healthcare provider can provide personalized recommendations for home safety.
How can I ensure proper home safety and fall prevention measures to reduce the risk of experiencing a periprosthetic fracture at home?
Implementing home safety measures such as removing tripping hazards, installing grab bars, and using assistive devices can help reduce the risk of falls and subsequent fractures. Your healthcare provider can provide personalized recommendations for home safety.
Are there specific activities or movements I should avoid to minimize the risk of experiencing a periprosthetic fracture after surgery?
Your healthcare provider may provide specific guidelines on activities to avoid or modify to reduce the risk of periprosthetic fractures. Following these recommendations can help protect your hip replacement and promote optimal healing
What should I do if I have concerns about the stability or integrity of my hip replacement implant following a periprosthetic fracture?
If you have concerns about the stability or integrity of your hip replacement implant, it’s important to discuss them with your healthcare provider. Additional imaging or evaluation may be necessary to assess the implant and determine the appropriate course of action.
How can I best prepare for the possibility of experiencing a periprosthetic fracture, both mentally and physically?
Mental and physical preparation for the possibility of a periprosthetic fracture involves understanding the risks, adhering to postoperative precautions, maintaining overall health, and having a support network in place. Open communication with your healthcare team can also help alleviate concerns and prepare for potential challenges.

