Hip and knee joint replacement surgeries are one of the most successful surgeries in the history of modern medicine. The surgeries relieve the pain and disability caused by arthritis not amicable by conservative management options. But like all surgeries, there is are risks of a number of complications after any hip or knee joint replacement surgery. The infection of the artificial joint is one of the dreaded complications of joint replacement.
The risk of infection after joint replacement surgery is roughly about 1% (1 in 100). The chances of infection are significantly higher in the case of revision surgery. The infection may develop in the tissues around the artificial joint or over the wound.
The infection may occur immediately in the hospital or after the patient goes home. Joint replacement infections may also develop years after the procedure.
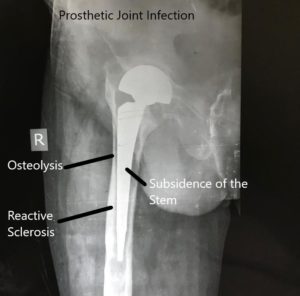
X-ray showing infected hip prosthetic joint.
Risk Factors
Active infection at the time of surgery is a significant risk factor for the development of artificial joint infection. The active infection may be present in the blood known as septicemia. The patient may also have an active infection in the local tissues such as skin, subcutaneous tissue, or deeper tissues. A history of prior local surgery or local infection increases the risk of infection.
Patients on immunosuppressant medications have an increased risk of prosthetic joint infection. Immunosuppressant medications decrease the body’s ability to fight back infections. This may lead to common microorganisms causing infection of the artificial joint.
Immunosuppressant drugs include chemotherapy drugs, corticosteroids, and disease-modifying drugs such as methotrexate. These drugs are often used in transplant recipients and cancer treatment.
Certain medical conditions decrease the body’s ability to fight infections. The diseases include uncontrolled diabetes mellitus, chronic kidney disease, liver failure, malnutrition, and HIV infection with low CD4 counts. Affected patients are at a higher risk of infection after joint replacement surgery.
Inflammatory medical conditions such as rheumatoid arthritis, psoriasis, and ankylosing spondylitis also increase the chances of prosthetic joint infection. Patients with a history of alcohol intake, smoking, iv drug abuse, and poor dental hygiene are at a greater risk of infection.

Prosthetic joint infection with redness of the overlying skin and swelling.
Causes of Joint Infections
There are several ways that bacteria, viruses, or fungi can sneak into your joints:
Direct Invasion: Sometimes, bacteria from an external wound or surgery site can travel through your bloodstream and settle into a joint, causing an infection. This is more common after joint replacement surgeries or injuries that break the skin.
Spread from Nearby Infections: Infections in surrounding tissues, such as bones or soft tissues, can spread to nearby joints if left untreated.
Medical Conditions: Certain medical conditions, like diabetes or autoimmune diseases, weaken your body’s defenses against infections, making you more susceptible to joint infections.
Invasive Procedures: Invasive medical procedures, such as injections into joints, can introduce bacteria into the joint space, leading to an infection.
Source
The bacteria residing normally in the skin is the most common cause of artificial joint infection. The microorganism may make it’s way to the joint through a sinus tract to the joint capsule. The dehiscence/giving away of the surgical wound may expose the deeper tissues to the external environment.
At times the microorganisms may infect the joint during the surgery. Strict precautions are taken to prevent intraoperative joint space infection. The infection may also occur by micro-organisms traveling through the blood. The organisms may get in the blood through infection anywhere in the body, dental procedures, ulcers, wound complications, etc.
Multiple local surgeries or a history of invasive procedures such as colonoscopy increase the chance of blood bacteremia.
Time of Infection
Acute or immediate infections occur within less than 90 days after the surgery. Commonly they occur within the first 3-6 weeks after the surgery. The infection is generally confined to the joint space only. The interface of the artificial component and the bone is usually not involved.
The infection occurring after 90 days is usually defined as a chronic infection. The infection may occur even years after the procedure. There is often a biofilm development. The development of biofilm also does not happen in the first 4 weeks.
The biofilm is produced by the infecting micro-organism. The biofilm acts as a barrier for the body’s defense mechanisms against infection.
Symptoms
The most common symptoms of prosthetic joint infection are persistent pain and stiffness of the involved joint. In acute infections, there may be additional symptoms of swelling, drainage of the joint, and joint tenderness. The symptoms may include low-grade fever and malaise.
Chronic infections may have very subtle presentations. The common symptoms are worsening of pain over a period of time. The patient may also experience progressive deterioration of the function of the involved joint.
The diagnosis of joint replacement infection involves a myriad of investigations involving radiological, blood, and joint aspirations. A complete assessment of the patient joint and health conditions is made by the consulting orthopedic surgeon.
The management of prosthetic joint infections is mostly surgical. The type of surgical management depends on multiple factors. Factors such as patient’s health, time since the joint replacement, and the severity of the infection may dictate the management.
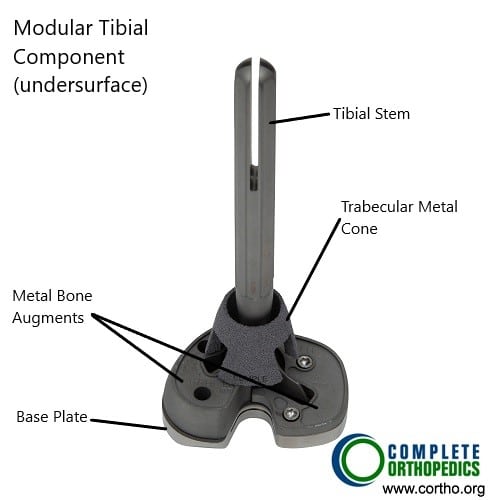
Modular tibial component with stem, metaphyseal cone and metal bone augments

Modular tibial component with stem
The above images show a modular tibial component that may be used in a revision knee replacement for an infected primary knee replacement. The modular component allows attachment of a stem and bone augments. The stem ensures rigid fixation and distribution of forces acting on the tibial base plate. The metaphyseal cone shown in the image has a coating mimicking the trabecular bone that allows biological fixation. Metal bone augments may be used to fill in the bone gaps encountered intraoperatively.
Do you have more questions?
Can joint replacement infections occur years after the surgery, or do they typically manifest shortly after?
Joint replacement infections can occur at any time post-surgery, ranging from days to years after the initial procedure.
Are certain individuals at higher risk of developing joint replacement infections than others?
Yes, individuals with preexisting conditions such as diabetes, obesity, compromised immune systems, or a history of previous joint infections may be at higher risk.
What are the typical symptoms of a joint replacement infection, and how do they differ from normal post-operative symptoms?
Symptoms of a joint replacement infection may include increased pain, swelling, warmth, redness, fever, chills, and wound drainage, which may persist or worsen despite initial healing.
Are there any specific laboratory tests or imaging studies used to diagnose joint replacement infections?
Yes, diagnostic tests may include blood tests (such as C-reactive protein and erythrocyte sedimentation rate), joint aspiration for culture and analysis, and imaging studies such as X-rays, MRI, or CT scans.
What is the typical course of treatment for a joint replacement infection?
Treatment often involves a combination of antibiotics, surgical debridement or irrigation, and in some cases, removal and revision of the infected implant.
Can joint replacement infections be effectively treated with antibiotics alone, or is surgical intervention usually necessary?
In most cases, surgical intervention is necessary to fully eradicate the infection, as antibiotics alone may not penetrate the biofilm or reach sufficient concentrations within the joint space.
How long does treatment for a joint replacement infection typically last, and what is the expected recovery time?
Treatment duration can vary depending on the severity of the infection and the chosen approach, but it may involve several weeks to months of antibiotic therapy and rehabilitation.
What are the potential complications or sequelae of a joint replacement infection, both in the short term and long term?
Complications may include persistent infection, implant failure, loss of function, chronic pain, joint stiffness, and the need for additional surgeries or revisions.
Can joint replacement infections spread to other parts of the body, and what are the implications of systemic spread?
Yes, joint replacement infections can potentially spread to surrounding tissues, bones, or the bloodstream, leading to systemic complications such as sepsis, organ failure, or secondary infections.
Are there any preventive measures that can reduce the risk of developing a joint replacement infection?
Yes, preventive measures may include proper surgical technique, antibiotic prophylaxis, preoperative optimization of medical conditions, and patient education on wound care and infection signs.
What is the role of perioperative antibiotics in preventing joint replacement infections, and how long are they typically administered?
Perioperative antibiotics are often given to reduce the risk of infection, with the duration varying based on factors such as surgical approach, patient comorbidities, and implant type.
Can joint replacement infections be prevented through lifestyle changes, such as weight loss or smoking cessation?
While lifestyle modifications such as weight loss and smoking cessation may improve overall health and reduce some risk factors, they may not completely eliminate the risk of joint replacement infections.
Is there a correlation between the type of implant used in joint replacement surgery and the risk of infection?
There is ongoing research into whether certain implant materials or designs may influence infection rates, but no definitive conclusions have been reached.
Are there any alternative treatments or adjunctive therapies being investigated for the management of joint replacement infections?
Research into alternative treatments such as antimicrobial coatings, biofilm disruptors, and immunomodulatory agents is ongoing, but their efficacy and safety are still being evaluated.
Can joint replacement infections lead to long-term joint damage or compromise the success of future revision surgeries?
Yes, joint replacement infections can lead to bone loss, soft tissue damage, and compromised joint function, which may complicate subsequent revision surgeries and affect outcomes.
How does the risk of joint replacement infection compare between primary joint replacement surgeries and revision surgeries?
Revision surgeries carry a higher risk of infection due to factors such as preexisting scar tissue, compromised soft tissues, and altered anatomy.
Are there any specific guidelines or recommendations for managing joint replacement infections in immunocompromised patients?
Management of joint replacement infections in immunocompromised patients may require a multidisciplinary approach involving infectious disease specialists, immunologists, and orthopedic surgeons, with tailored antibiotic regimens and close monitoring.
What is the likelihood of recurrence after successfully treating a joint replacement infection, and are there ways to minimize this risk?
The likelihood of recurrence varies depending on factors such as the underlying cause of the infection, the effectiveness of treatment, and patient-specific factors. Minimizing risk may involve optimizing overall health, addressing modifiable risk factors, and vigilant follow-up care.

Dr. Mo Athar
[et_pb_button admin_label="Button" button_url="https://www.cortho.org/general-appointment/" url_new_window="off" button_text="Schedule an Appointment" button_alignment="center" background_layout="light" custom_button="on" button_text_color="#FFFFFF" button_bg_color="#02770B" button_border_color="#FFFFFF" button_letter_spacing="1" button_font="Arial" button_on_hover="on" button_text_color_hover="#FFFFFF" button_bg_color_hover="#02770B" button_letter_spacing_hover="1" /]
