Osteoporosis is a condition that leads to the weakening of bones due to the loss of both calcium and protein in the bone matrix. This makes the bones more fragile and increases the risk of fractures, often without a clear cause. The condition worsens with age, and it is particularly common among postmenopausal women. It is estimated that about 50% of women and 25% of men over the age of 50 experience decreased bone density, making them susceptible to fragility fractures, including vertebral compression fractures.
Functional Anatomy
The spine is composed of a series of vertebrae that protect the spinal cord and support the body’s weight. The vertebrae are interconnected by discs that act as cushions, preventing the bones from rubbing against each other. The vertebral bodies, which are the large, round parts of the vertebrae, bear most of the weight. In osteoporosis, these vertebrae become weaker and can collapse under pressure, leading to vertebral compression fractures.
Biomechanics or Physiology
Forces and loads are transferred through the spine, and vertebrae play a central role in absorbing and distributing these forces. Healthy vertebrae maintain their shape and structural integrity, allowing them to withstand the weight and movement of the body. However, in individuals with osteoporosis, the vertebral bodies lose strength, leading to the collapse of the vertebrae under normal body weight and strain, resulting in fractures.
Osteoporosis Indications
Patients who have multiple compression fractures had no relief with conservative measures. Occasionally patients with malignancy like metastases or multiple myeloma of the vertebral body with pain can be a candidate for vertebroplasty or kyphoplasty.
Osteoporosis Contraindications
Patients who have multiple vertebral involvements, severe osteoporosis, vertebral segment instability, and neurological deficits are contraindications for this procedure.
Common Variants and Anomalies
Vertebral fractures can occur at various points along the spine but are most commonly found in the thoracic and lumbar regions. These fractures may happen gradually over time or can be triggered by an event such as a fall. The condition can vary in severity, from mild fractures that cause no symptoms to more severe ones that can lead to significant pain and disability.
Clinical Relevance
Osteoporotic vertebral compression fractures are a significant cause of pain and disability in older adults. They often lead to a decreased ability to perform daily activities, and the pain can affect the quality of life. The fractures may occur without a major injury, and the condition is frequently undiagnosed until symptoms arise. Vertebral fractures in osteoporosis can also cause deformities like kyphosis (a curvature of the spine), which can further affect posture and mobility.
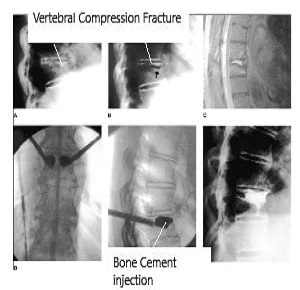
Imaging Overview
X-rays and MRIs are commonly used to diagnose vertebral compression fractures. X-rays can reveal the extent of the fracture and any changes in vertebral height. MRI can provide more detailed images of the soft tissues, including the spinal cord, and is helpful in ruling out other causes of pain, such as tumors or infections. In some cases, CT scans may be used for more detailed imaging of the bone structure.
Associated Conditions
Vertebral compression fractures are closely associated with osteoporosis, particularly in postmenopausal women. Other conditions, such as multiple myeloma, metastatic cancer, and other forms of bone weakening, can also lead to vertebral fractures. Additionally, conditions that affect the spinal alignment or increase the risk of falls, such as balance disorders, may exacerbate the likelihood of these fractures.
Surgical or Diagnostic Applications
Surgeons use imaging techniques to assess the severity of vertebral fractures and to plan the most appropriate treatment. For patients with persistent pain or those whose fractures do not heal with conservative treatments, vertebroplasty or kyphoplasty may be recommended. These procedures involve injecting bone cement into the fractured vertebra to stabilize the bone and relieve pain. In kyphoplasty, a balloon is first used to restore the height of the vertebra before the cement is injected.
Osteoporosis Procedure
Appropriately chosen patients are worked up by the use of x-ray and MRI. Occasionally, CT scan may be needed. Patients who need vertebroplasty or kyphoplasty are taken to the operating room. The procedure is usually done under general anesthesia but can also be performed under local anesthesia.
Patients are placed prone on the operating table. Intraoperative x-rays or fluoroscopy is used. The procedure is performed through a pinpoint incision through which a hollow needle is passed from the skin into the vertebral body. The location is checked under x-ray imaging.
Once the needle is in the right phase, the vertebra is filled with bone cement if only vertebroplasty is performed. In contrast, for kyphoplasty, a balloon is inflated within the vertebral body to restore the height of the vertebra. Then, bone cement is injected to fill the cavity. The needle is removed before the bone cement hardens.
Once the procedure is over, the patient is flipped onto the back and sent to a recovery room. Most patients are discharged from recovery. Patients are allowed to walk with or without the use of brace after the procedure. Patients are also given some pain medications and are followed in the office.
Results And Prognosis
In appropriately chosen patients, vertebroplasty and kyphoplasty are big procedures which are done essentially for pain relief. They can also help restore vertebral height. They gave adequate pain relief in patients with metastasis or multiple myeloma. Vertebroplasty and kyphoplasty help in decreasing pain, improving quality of life, and decreasing mortality. Vertebroplasty can also be used in patients with pain due to hemangioma of the vertebrae.
Prevention and Maintenance
Preventing osteoporotic vertebral fractures involves addressing bone health early. Weight-bearing exercises, a diet rich in calcium and vitamin D, and medications that improve bone density can help reduce the risk of fractures. Posture training and fall prevention strategies, including balance exercises, are also important for individuals at risk. It is crucial for those with osteoporosis or a history of fractures to work with their healthcare providers to develop a plan for maintaining bone health.
Research Spotlight
A recent study evaluated the effectiveness of third-generation vertebral augmentation systems (TVA) for treating osteoporotic vertebral compression fractures (OVCFs) in comparison with other methods such as percutaneous kyphoplasty (PKP) and vertebroplasty (PVP).
The network meta-analysis demonstrated that TVA offered superior short-term outcomes, significantly reducing pain, improving functional disability, and enhancing quality of life compared to non-surgical management (NSM). In long-term follow-ups, TVA maintained its advantage in reducing disability, although PKP excelled in preserving vertebral body height.
Importantly, TVA demonstrated a lower risk of adverse events such as bone cement leakage (BCL) and adjacent vertebral fractures (AVF) compared to PKP and PVP. The study underscores the promising safety and efficacy profile of TVA for OVCFs, though further high-quality trials with extended follow-up are needed to confirm these findings (“Study on third-generation vertebral augmentation systems for OVCFs – See PubMed“).
Summary and Key Takeaways
Osteoporotic vertebral compression fractures are a common and debilitating condition, particularly affecting older adults. They occur when weakened vertebrae collapse under pressure, leading to pain and reduced mobility. Vertebroplasty and kyphoplasty are effective surgical treatments for managing these fractures when conservative measures fail. Preventing osteoporosis through bone health maintenance and fall prevention is essential in reducing the risk of fractures. Regular screening and early intervention are key to managing this condition effectively.
For Kyphoplasty and Vertebroplasty priocedure and cost information, please click here.

