Total disc replacement (TDR) is a surgical procedure designed to replace a damaged intervertebral disc with an artificial prosthetic disc, restoring the spine’s mobility and alleviating pain. It is performed primarily in the cervical and lumbar regions of the spine, where degenerative disc disease or herniated discs cause significant pain and disability.
How Common It Is and Who Gets It? (Epidemiology)
Disc degeneration and herniation are common causes of back and neck pain. A growing number of patients are undergoing total disc replacement, particularly those with persistent symptoms of radiculopathy from a herniated or damaged disc that has not responded to conservative treatments. Most candidates for TDR are between the ages of 30 and 60, with a higher prevalence in individuals involved in manual labor or those with sedentary lifestyles contributing to spinal wear and tear.
Why It Happens – Causes (Etiology and Pathophysiology)
The intervertebral disc is a gel-like structure that cushions the vertebrae and allows for spinal mobility. Over time, wear and tear, trauma, or degenerative changes, such as decreased hydration in the disc’s nucleus pulposus, can lead to disc herniation or bulging. These conditions compress nearby nerve roots or the spinal cord, causing pain, weakness, numbness, and in severe cases, loss of mobility. Obesity, smoking, poor posture, and repetitive strain are contributing factors to disc degeneration and herniation.

Axial section of the cervical spine showing disk herniation on MRI.
How the Body Part Normally Works? (Relevant Anatomy)
The intervertebral discs are located between the vertebrae and serve as shock absorbers, allowing the spine to flex, extend, and rotate. Each disc consists of two parts: the nucleus pulposus, a gel-like center, and the annulus fibrosus, the tough outer ring. The discs also maintain the space between vertebrae, enabling the nerve roots to exit the spinal cord without compression.
What You Might Feel – Symptoms (Clinical Presentation)
Symptoms of a damaged or herniated disc can include sharp, radiating pain in the neck or lower back, which may extend down the arms or legs. Patients often experience tingling, numbness, or weakness in the affected limbs. In more severe cases, patients may suffer from reduced mobility, and in extreme cases, motor deficits or bowel and bladder dysfunction may occur.
How Doctors Find the Problem? (Diagnosis and Imaging)
Diagnosis is confirmed through clinical examination and imaging studies. An MRI is the gold standard for identifying disc herniation, disc degeneration, and nerve root compression. In cases of cervical or lumbar pain, MRI scans will reveal the location and extent of the herniation, the condition of the discs, and any impingement on the nerves or spinal cord.
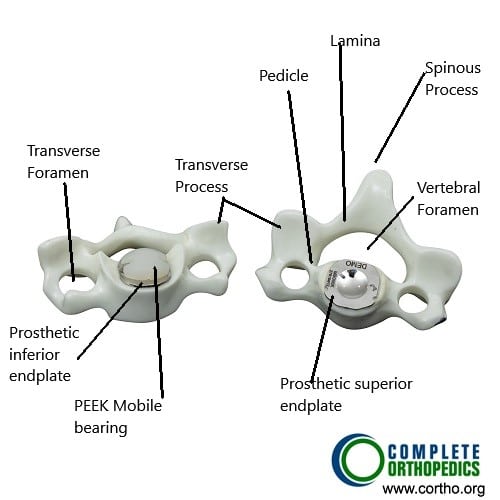
The image above shows a total cervical disc replacement along with various parts of the cervical vertebra. The components of the total cervical disc replacement include metal parts attached on the adjoining vertebrae to create the space for the prosthetic disc. The prosthetic disc is usually made of a PEEK (poly-ether-ether-ketone) polymer.
Classification
Total disc replacement is typically indicated for patients with single-level or multi-level disc degeneration or herniation. Candidates must have no significant facet joint arthritis or spinal instability, as these conditions could complicate the procedure. TDR is classified based on the location of the disc herniation—cervical or lumbar—and the type of prosthetic disc used.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that can mimic the symptoms of disc herniation include facet joint arthritis, spinal stenosis, piriformis syndrome, and muscle strains. Infections or tumors in the spine can also present with similar symptoms, necessitating a thorough work-up to rule out other conditions.
Treatment Options
Non-Surgical Care
Conservative treatment for disc herniation includes physical therapy, anti-inflammatory medications (NSAIDs), heat or cold therapy, and spinal injections such as epidural steroid injections. If conservative methods fail, surgical intervention may be considered, with TDR as an option for suitable candidates.
Surgical Care
Total disc replacement involves the removal of the damaged disc and insertion of an artificial disc to maintain motion at the affected segment. Other surgical options include spinal fusion, but fusion does not preserve motion in the affected segment, which TDR aims to do.
Recovery and What to Expect After Treatment
Postoperative recovery for total disc replacement generally takes about 6 weeks, with patients gradually returning to normal activities. During the rehabilitation period, patients focus on strengthening the muscles around the spine to support the new disc. Most patients report a significant reduction in pain and improvement in function.
Possible Risks or Side Effects (Complications)
As with any surgery, total disc replacement carries potential risks, including infection, bleeding, nerve injury, implant failure, and the development of adjacent segment disease (additional degeneration in nearby discs). Long-term complications could include disc displacement or wear and tear of the prosthetic.
Long-Term Outlook (Prognosis)
The prognosis for patients undergoing TDR is generally positive, with most patients experiencing significant pain relief and restored mobility. However, the long-term success of the procedure depends on factors such as the quality of the implant, patient adherence to rehabilitation, and the absence of other spinal diseases.
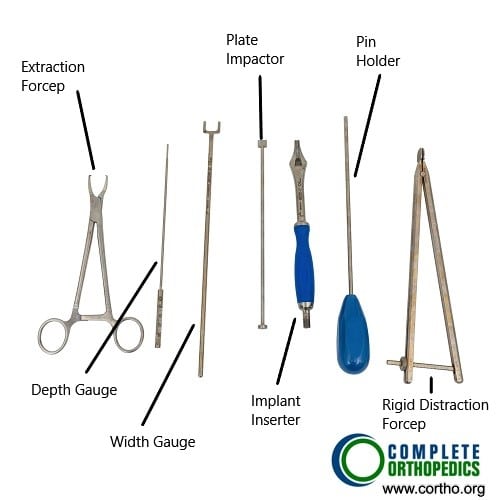
The instruments shown in the image above are used during the surgery to remove the diseased disc, create raw bone surface for implanting the metal endplates and subsequent insertion of the prosthetic disc.
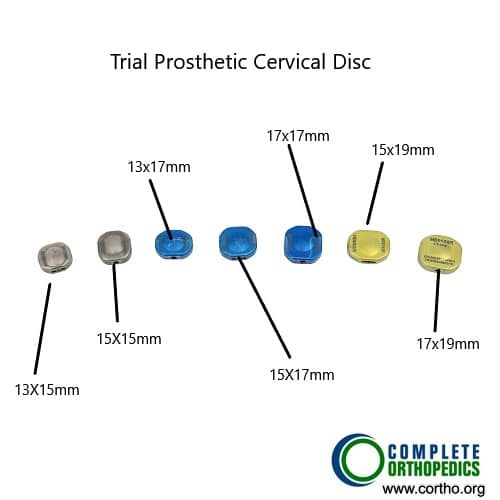
The trial cervical discs are used to find the correct size of the final cervical prosthetic disc for maximum stability and motion.
Out-of-Pocket Costs
Medicare
CPT Code 22856 – Cervical Total Disc Replacement (Single Level): $396.11
CPT Code 22857 – Lumbar Total Disc Replacement: $412.08
Under Medicare, 80% of the approved amount for these procedures is covered once the annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—usually cover this 20%, leaving most patients with little to no out-of-pocket expenses for Medicare-approved disc replacement surgeries. These supplemental plans work directly with Medicare to ensure full coverage for the procedure.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it serves as a secondary payer once Medicare processes the claim. After your deductible is satisfied, these secondary plans may cover any remaining balance, including coinsurance or any uncovered charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on the specific policy and network status.
Workers’ Compensation
If your cervical or lumbar disc replacement surgery is work-related, Workers’ Compensation will fully cover all treatment-related costs, including the procedure, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your cervical or lumbar spine injury resulting in total disc replacement is caused by a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses, including disc replacement surgery. The only possible out-of-pocket expense may be a small deductible depending on your individual policy terms.
Example
John, a 62-year-old patient with severe cervical disc degeneration, required cervical total disc replacement (CPT 22856). His estimated Medicare out-of-pocket cost was $396.11. Since John had supplemental insurance through Blue Cross Blue Shield, the 20% not covered by Medicare was fully paid, leaving him with no out-of-pocket expenses for the surgery.
Frequently Asked Questions (FAQ)
Q. What is the recovery time after total disc replacement?
A. Most patients can return to normal activities within 6 weeks, although a full recovery may take up to 3 months.
Q. Is total disc replacement suitable for everyone?
A. Not all patients are candidates. Those with osteoporosis, inflammatory spine diseases, or significant spinal instability are generally not considered for TDR.
Q. What are the risks of total disc replacement?
A. Risks include infection, nerve damage, implant failure, and adjacent segment degeneration. It is important to discuss all potential risks with your surgeon.
Summary and Takeaway
Total disc replacement is an effective option for patients with herniated or degenerative discs who are seeking to maintain spinal mobility and alleviate pain. While the procedure is successful for many patients, it is not suitable for everyone. Proper patient selection and thorough preoperative evaluation are critical to achieving the best outcomes.
Clinical Insight & Recent Findings
A recent study explored the combined use of total disc replacement (TDR) and the Total Posterior Facet Replacement System (TOPS) as a potential solution for treating degenerative spine disorders. The study highlights how TDR, which preserves motion by replacing damaged intervertebral discs, can be complemented by the TOPS device, designed to address deficiencies in the posterior spinal column.
This combination is FDA-approved for individual use but has not yet been tested for combined application. The study raises important considerations regarding biomechanical compatibility, clinical indications, and costs before widespread adoption of this combined approach.
These devices, while not specifically tailored for combined use, may offer significant advantages for motion preservation and could serve as a bridge in spinal treatment until biological therapies become viable (“Study on combined TDR and TOPS system – See PubMed“).
Who Performs This Treatment? (Specialists and Team Involved)
Total disc replacement is performed by orthopedic surgeons or neurosurgeons specializing in spinal surgery. A multidisciplinary team, including physical therapists, anesthesiologists, and rehabilitation specialists, is often involved in the patient’s care.
When to See a Specialist?
You should see a specialist if you experience persistent neck or back pain, particularly if it radiates to the arms or legs, and if conservative treatments have not been effective. A specialist will help determine whether total disc replacement is appropriate.
When to Go to the Emergency Room?
Seek emergency care if you experience sudden weakness, numbness, or loss of bowel or bladder control, as these may indicate a more serious spinal problem requiring urgent attention.
What Recovery Really Looks Like?
Patients typically experience significant improvement in pain and function within 6 weeks. However, full recovery can take up to 3 months, depending on the individual and the specific surgery.
What Happens If You Ignore It?
Ignoring disc herniation or degeneration can lead to chronic pain, nerve damage, and loss of mobility. In some cases, untreated conditions may result in permanent neurological deficits.
How to Prevent It?
Maintaining good posture, regular exercise, and a healthy weight can help prevent disc degeneration. Avoid heavy lifting and repetitive activities that place stress on the spine.
Nutrition and Bone or Joint Health
A diet rich in calcium and vitamin D, along with regular exercise, can help maintain spinal health and prevent degenerative conditions. Proper hydration is also crucial for disc health.
Activity and Lifestyle Modifications
To prevent further strain on the spine, avoid prolonged sitting, heavy lifting, and activities that may aggravate back or neck pain. Low-impact exercises, such as swimming or walking, can strengthen the spine and reduce the risk of future injuries.
Do you have more questions?
What materials are used in artificial discs?
Artificial discs are typically made from metal alloys such as titanium or cobalt-chromium and a medical-grade plastic called polyethylene. These materials are chosen for their strength, durability, and compatibility with the human body, ensuring they can withstand the stresses of daily activities
What are the chances of needing additional surgery after CTDR?
The likelihood of needing additional surgery is lower with CTDR compared to spinal fusion, especially concerning adjacent segment disease. However, some patients might still require further surgical interventions if complications arise or symptoms persist
Are there any activities I should avoid after CTDR?
Initially, you should avoid heavy lifting, repetitive neck movements, and high-impact activities. Your surgeon will provide specific guidelines based on your recovery progress. Gradually, you will be able to resume most activities as your neck heals
How does CTDR compare to spinal fusion in terms of pain relief?
Studies have shown that CTDR provides comparable, if not superior, pain relief compared to spinal fusion. Additionally, CTDR has the added benefit of preserving spinal motion, which can lead to better overall outcomes
What are the long-term outcomes of CTDR?
Long-term studies show that CTDR provides sustained pain relief and functional improvement, maintaining motion at the treated segment. Patients typically experience a reduced need for additional surgery compared to those who undergo spinal fusion. This is due to the preservation of natural spinal motion, which helps to reduce stress on adjacent discs
Is CTDR suitable for elderly patients?
Age alone does not disqualify someone from CTDR. However, the overall health and bone quality of elderly patients must be considered. Conditions like osteoporosis might affect the stability of the implant. A comprehensive evaluation by a spine specialist will help determine if CTDR is appropriate
Can CTDR be performed if I have osteoporosis?
Severe osteoporosis can affect bone integrity and stability of the implant, making CTDR less feasible. Each case needs to be evaluated individually, and other treatment options may be considered if osteoporosis is present
Can I drive after CTDR surgery?
You can typically resume driving once you are off pain medications and can comfortably and safely turn your head. This is usually within a few weeks post-surgery. However, it’s important to follow your surgeon’s specific advice on this matter
What are the potential complications specific to CTDR?
Specific complications can include device dislocation, subsidence (sinking of the device into the vertebrae), and wear of the artificial disc. Although these complications are relatively rare, they can require additional surgical intervention if they occur
How does CTDR affect overall spinal alignment?
CTDR aims to maintain or restore normal spinal alignment and curvature, potentially reducing the risk of further spinal issues
Are there non-surgical alternatives to CTDR for cervical disc disease?
Non-surgical treatments include physical therapy, medications, injections, and lifestyle modifications. Surgery is considered when these treatments fail to provide adequate relief
How do I choose the right surgeon for CTDR?
Look for a board-certified spine surgeon with extensive experience in performing CTDR. Check their credentials, patient reviews, and success rates with this specific procedure
What advancements are being made in CTDR technology?
Ongoing advancements include improved biomaterials, design enhancements for better motion preservation, and minimally invasive surgical techniques to reduce recovery time

