Revision spine surgery is a procedure performed on patients who have previously undergone spine surgery, but the results did not meet expectations. These surgeries are typically more complex than the original spine surgeries and are done to correct issues such as re-herniation of discs, failed fusion, or hardware complications. Revision surgery can be performed on both the cervical and lumbar regions of the spine.
How Common It Is and Who Gets It? (Epidemiology)
Revision spine surgeries are not uncommon, particularly in patients who have undergone spinal procedures such as disc replacements, spinal fusions, or laminectomies. Factors such as poor healing, re-herniation of discs, infection, or failure of hardware can necessitate a second surgery. Patients who suffer from chronic conditions such as diabetes, obesity, or immune system disorders are at a higher risk for requiring revision surgery due to poor healing. Smoking also significantly increases the risk of surgical failure.
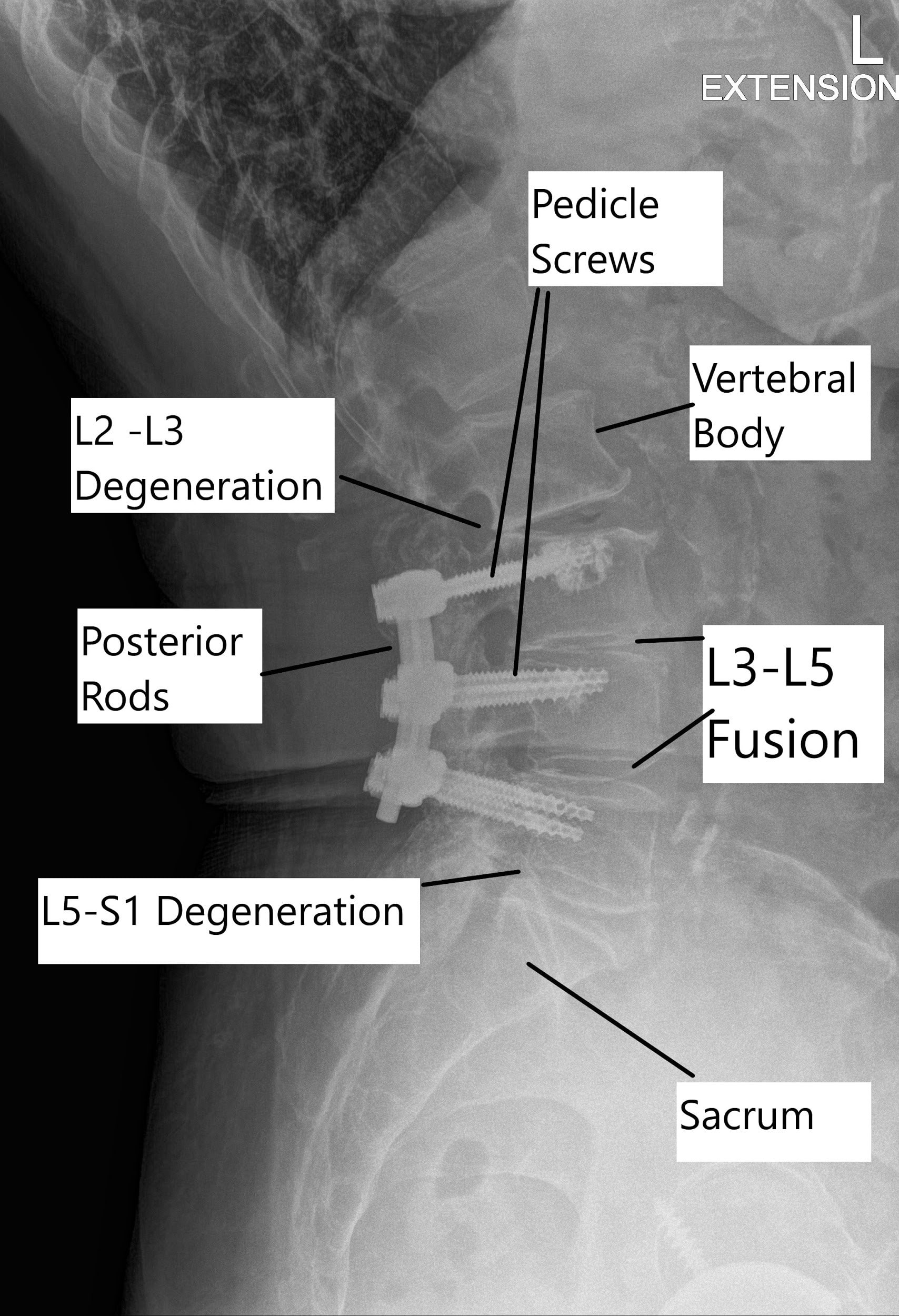
Status post L3 to L5 fusion with adjacent segment degeneration of L2-3 and L5-S1 on X-ray.
Why It Happens – Causes (Etiology and Pathophysiology)
The need for revision spine surgery typically arises due to a failure of the original surgery. In the case of fusion surgery, failure can occur if the bones do not fuse properly (pseudoarthrosis), resulting in the loosening of screws or rods. Other causes include infection, adjacent segment degeneration, or failure of the implanted hardware. The failure of fusion is more common in patients with medical conditions such as diabetes, kidney disease, and smoking. Poor patient selection or incorrect surgical techniques can also lead to the need for revision surgery.
How the Body Part Normally Works? (Relevant Anatomy)
The spine is composed of vertebrae separated by intervertebral discs, which act as cushions. In spine surgery, the goal is often to alleviate pressure on nerves or stabilize the spine. A spinal fusion procedure involves joining two or more vertebrae together to prevent movement at the affected segment. When this fusion fails, the vertebrae may shift, causing additional pain or nerve compression. Adjacent segment degeneration occurs when the vertebrae adjacent to a fusion site begin to deteriorate due to increased stress from the lack of motion in the fused segments.
Failed back surgery syndrome
A failed back surgery syndrome is the persistence of the chronic symptoms of pain after one or more surgeries of the spine. The failed back surgery syndrome occurs when the outcome of the surgery is not as expected by the patient or the surgeon.
Spine surgery performed in patients in whom the surgery was not indicated or poor patient selection is the most common cause of failed back surgery. Other causes of failed spine surgery include patients with an incorrect/incomplete initial diagnosis, wrong procedure/technique, chronic smokers, and patients with immune-suppressing co-morbid diseases. Postoperative complications such as a dural tear, infection, or hematoma may lead to failed back syndrome.
What You Might Feel – Symptoms (Clinical Presentation)
Patients who require revision spine surgery often present with symptoms such as persistent pain, numbness, weakness, and loss of function that continue after the initial surgery. Other signs may include pain at the site of previous surgery, neurological deficits due to nerve compression, or instability in the spine. Patients may also experience signs of infection or hardware failure, such as fever or increased swelling at the surgical site.
Time of appearance of symptoms
An early appearance of symptoms immediately after surgery or within 2-3 weeks after surgery may most commonly result from a wrong level of surgery, inadequate diagnosis, or procedure. The symptoms appearing after one month up to a period of six months may result from graft or implant failure or from recurrent disc herniation. After six months, symptoms may result from recurrent stenosis at the same or a different level or from excessive scar tissue formation.
Transition syndrome results from the instability of the segments adjoining the fused segment in surgery. The additional stress on the adjoining segment due to the successful fusion of diseased level may result in accelerated degenerative changes in the adjoining level.
How Doctors Find the Problem? (Diagnosis and Imaging)
The diagnosis of failed spine surgery involves a detailed history, physical examination, and imaging studies. Initial radiological tests usually include X-rays to assess the alignment of the spine and the position of any implants. If these show signs of failure, further imaging with MRI or CT scans may be performed to evaluate the soft tissues, spinal cord, and nerve roots. These tests help to identify complications such as re-herniation, infection, or hardware failure.
Classification
Revision spine surgery can be classified based on the type of complication that led to the revision. Common classifications include:
- Failed fusion: Inadequate healing of the vertebrae after a fusion procedure.
- Adjacent segment degeneration: Degeneration of vertebrae next to a previously fused segment.
- Hardware failure: Loosening or breakage of screws, rods, or cages used in the original surgery.
- Infection or scarring: Complications arising from infection or excessive scar tissue formation.
- Recurrent disc herniation: A herniated disc that reappears after initial surgery.
Other Problems That Can Feel Similar (Differential Diagnosis)
Conditions that may present similarly to failed spine surgery include muscle strain, ligament sprains, or arthritis. Additionally, other issues such as tumors, infections, or vascular problems can cause back or neck pain, and these must be ruled out during the diagnostic process.
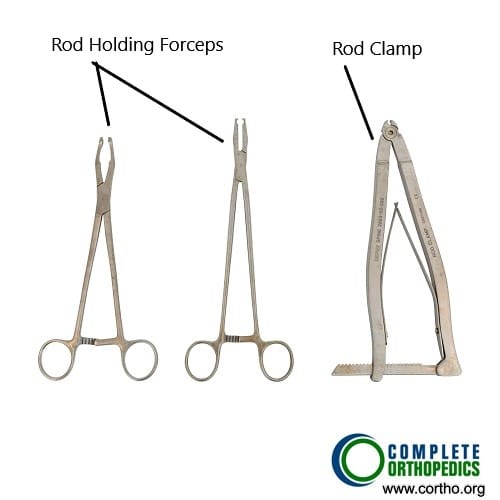
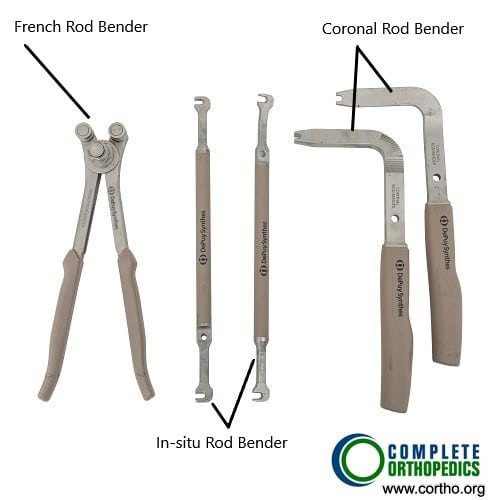
The images above show various types of instruments used in posterior spinal fusion which may be used for revision surgery. The rods are used to stabilize the spinal segments and are tightened over the pedicle screws. The rods may be contoured to a required shape during the surgery to achieve maximum stability using the rod benders.
Treatment Options
Non-Surgical Care
Initially, conservative treatments such as pain management, physical therapy, and epidural steroid injections may be attempted. These methods can help alleviate pain and improve mobility in some cases. For patients with minor symptoms or instability, non-invasive treatments may be sufficient.
Surgical Care
When conservative methods fail or if significant instability or nerve compression is present, revision surgery is necessary. This surgery typically involves removing the failed hardware, cleaning the fusion site, and inserting new bone grafts and implants. The goal is to restore stability, relieve nerve pressure, and address any other issues causing persistent symptoms.
Recovery and What to Expect After Treatment
Recovery from revision spine surgery varies depending on the complexity of the procedure and the patient’s overall health. Many patients experience a shorter hospital stay compared to the original surgery, but the recovery process can take several months. Physical therapy is often recommended to help restore strength and mobility. Postoperative care includes managing pain, preventing infection, and monitoring for complications such as blood clots or nerve issues.
Possible Risks or Side Effects (Complications)
As with any surgery, revision spine surgery carries risks, including:
- Infection
- Bleeding
- Nerve damage
- Failure of the new fusion or hardware
- Adjacent segment degeneration
- Chronic pain or recurrence of symptoms
Certain patient populations, such as smokers or those with diabetes, may be at higher risk for complications.
Long-Term Outlook (Prognosis)
The prognosis after revision spine surgery is generally positive for most patients, particularly if the original surgery failed due to factors that can be corrected with revision. Many patients experience significant relief from pain and improved function, though long-term outcomes depend on the cause of failure, the patient’s overall health, and adherence to postoperative care.
Out-of-Pocket Costs
Medicare
CPT Code 22830 – Revision Spine Surgery: $201.32
CPT Code 22852 – Removal of Posterior Segmental Instrumentation: $173.63
Under Medicare, 80% of the approved amount for these procedures is covered once your annual deductible has been met. The remaining 20% is typically the patient’s responsibility. Supplemental insurance plans—such as Medigap, AARP, or Blue Cross Blue Shield—usually cover this 20%, leaving most patients with little to no out-of-pocket expenses for Medicare-approved spine surgeries. These supplemental plans work directly with Medicare to ensure full coverage for the procedures.
If you have secondary insurance—such as Employer-Based coverage, TRICARE, or Veterans Health Administration (VHA)—it acts as a secondary payer once Medicare processes the claim. After your deductible is satisfied, the secondary plan may cover any remaining balance, including coinsurance or any uncovered charges. Secondary plans typically have a modest deductible, usually between $100 and $300, depending on the policy and network status.
Workers’ Compensation
If your revision spine surgery or removal of instrumentation is work-related, Workers’ Compensation will fully cover all treatment-related costs, including surgery, hospitalization, and rehabilitation. You will have no out-of-pocket expenses under an accepted Workers’ Compensation claim.
No-Fault Insurance
If your spine condition requiring revision surgery or instrumentation removal is caused by a motor vehicle accident, No-Fault Insurance will cover all medical and surgical expenses. The only possible out-of-pocket cost may be a small deductible depending on your specific policy terms.
Example
Susan, a 67-year-old patient with previous lumbar fusion requiring revision surgery (CPT 22830) and removal of posterior instrumentation (CPT 22852), had estimated Medicare out-of-pocket costs of $201.32 for the revision surgery and $173.63 for the instrumentation removal. Since Susan had supplemental insurance through Blue Cross Blue Shield, the 20% that Medicare did not cover was fully paid, leaving her with no out-of-pocket expenses for the surgeries.
Frequently Asked Questions (FAQ)
Q. What are the most common reasons for revision spine surgery?
A. The most common reasons are failed fusion, hardware failure, adjacent segment degeneration, and recurrent disc herniation.
Q. How soon after surgery can I expect to feel relief from symptoms?
A. Many patients feel relief from their symptoms within a few weeks, but full recovery can take several months.
Q. Can revision surgery be performed on both the cervical and lumbar spine?
A. Yes, revision surgery can be performed on both the cervical and lumbar regions of the spine, depending on the location of the original surgery and the complications.
Summary and Takeaway
Revision spine surgery is a necessary procedure for patients whose initial spine surgery has failed to provide the expected relief or has caused new issues. It involves more complexity than primary surgery, but with proper management, many patients experience significant improvements in pain and function. However, the risks of revision surgery are higher, and patients must work closely with their healthcare team to ensure a successful outcome.
Clinical Insight & Recent Findings
A recent study investigated a rare complication following revision spine surgery: the development of subdural hygroma, which can cause neurological deterioration. In the case described, a patient who underwent revision lumbar fusion developed conus medullaris syndrome and subdural fluid collection 10 days after surgery.
The condition was identified through MRI, which showed fluid accumulation at the T12-L2 level. Surgical intervention, including fluid evacuation and dural sac repair, resulted in significant neurological recovery.
This study highlights the importance of considering subdural hygroma as a potential cause of neurological symptoms after revision spine surgery, especially when motor weakness emerges postoperatively. (“Study of subdural hygroma after revision spine surgery – See PubMed.“)
Who Performs This Treatment? (Specialists and Team Involved)
Revision spine surgery is performed by orthopedic or neurosurgeons who specialize in spinal procedures. The surgical team may also include surgical assistants, anesthesiologists, and nursing staff trained in spine surgery.
When to See a Specialist?
If you experience ongoing pain, weakness, or numbness after a spine surgery, or if new symptoms develop, it is important to consult with a spine specialist. Early intervention can help prevent further complications and improve the outcome of any necessary revision surgery.
When to Go to the Emergency Room?
Seek emergency care if you experience severe chest pain, difficulty breathing, signs of stroke, or any other life-threatening symptoms after surgery.
What Recovery Really Looks Like?
Recovery from revision spine surgery involves gradual improvement in pain and mobility. Patients will likely need physical therapy to regain strength and flexibility, and they must follow the doctor’s guidelines to avoid complications.
What Happens If You Ignore It?
Ignoring symptoms of failure after spine surgery can lead to worsening pain, nerve damage, or permanent disability. Early revision surgery can prevent these long-term complications.
How to Prevent It?
Maintaining a healthy weight, avoiding smoking, and staying active with low-impact exercises can help prevent spine issues that may require surgery. Regular check-ups with a spine specialist are also recommended.
Nutrition and Bone or Joint Health
A healthy diet rich in calcium and vitamin D can support bone health and promote healing after spine surgery. Proper nutrition is essential for recovery and maintaining the health of your spine.
Activity and Lifestyle Modifications
After revision spine surgery, it is important to follow your surgeon’s advice regarding activity restrictions. Avoid heavy lifting, high-impact sports, and any activity that could stress the spine. Staying active with walking and gentle exercises can help in recovery.
Do you have more questions?
How is a patient evaluated for revision spinal surgery?
Evaluation includes a thorough medical history, physical examination, and imaging studies like X-rays, MRI, or CT scans to assess the condition of the spine and any complications from the initial surgery.
How long is the recovery time after revision spinal surgery?
Recovery can take several weeks to months, depending on the extent of the surgery and the individual patient’s healing process. Physical therapy is often required to aid recovery.
What is the success rate of revision spinal surgery?
Success rates vary, but many patients experience significant improvement. However, outcomes can be less predictable than with primary surgery, depending on the reason for revision and the patient’s overall health.
What can I do to prepare for revision spinal surgery?
Preparation includes discussing all medications with your surgeon, stopping certain drugs that could increase bleeding, and following any preoperative instructions given by your medical team.
How do I know if my symptoms are due to the failure of my initial surgery?
Symptoms like recurrent pain, neurological deficits, or changes in mobility may indicate issues with the initial surgery. A thorough evaluation by your surgeon is necessary to determine the cause.
What types of imaging studies are used to assess the need for revision surgery?
X-rays, MRI, and CT scans are commonly used to evaluate the spine’s condition, check for hardware issues, and identify any new or unresolved problems.
Is revision spinal surgery more painful than the first surgery?
Pain levels vary, but revision surgery can sometimes result in more postoperative discomfort due to the complexity of the procedure and the presence of scar tissue.
What are the chances of needing another surgery after a revision procedure?
While the goal is to address all issues during the revision, some patients may require further surgeries, especially if complications arise or new spinal problems develop.
How can I reduce the risk of complications after revision spinal surgery?
Follow your surgeon’s postoperative instructions carefully, attend all follow-up appointments, avoid smoking, maintain a healthy diet, and engage in recommended physical therapy.
What are the potential long-term outcomes of revision spinal surgery?
Long-term outcomes vary, but many patients experience pain relief and improved function. However, some may have ongoing symptoms or require further treatment.
Is it possible to prevent the need for revision spinal surgery?
While not all cases can be prevented, proper patient selection, careful surgical technique, and adherence to postoperative care can reduce the likelihood of requiring revision surgery.
How does scar tissue affect revision spinal surgery?
Scar tissue can complicate revision surgery by making it more difficult to access the surgical site and increasing the risk of complications like nerve damage or dural tears.
What is adjacent segment disease, and how is it related to revision spinal surgery?
Adjacent segment disease occurs when the segments of the spine above or below a fusion develop degenerative changes due to altered biomechanics. This condition may require revision surgery if symptoms become significant.
What questions should I ask my surgeon before undergoing revision spinal surgery?
Key questions include asking about the specific reasons for revision surgery, potential risks and benefits, the expected recovery process, the likelihood of success, and how the surgery will address your current symptoms.

