Total Knee Replacement
Anyone can experience knee discomfort from time to time. However, if the pain becomes severe, interferes significantly with your daily activities, or is accompanied by swelling, tenderness, or inflammation, it’s important to see a doctor.
At Complete Orthopedics, our team of specialized orthopedic knee experts is dedicated to treating knee pain with a range of treatments, including surgery if needed. We have locations in New York City and Long Island, and we perform surgeries at six hospitals, providing access to advanced knee surgery and orthopedic care. You can easily book an appointment with one of our orthopedic surgeons online or by phone.
Learn about common causes of knee pain and the treatment options available, including when surgery might be the best option.
Overview
Total knee replacement is a surgical procedure to replace the damaged parts of the knee joint with metal and plastic parts. It is one of the most common surgeries performed by orthopedic surgeons. Common causes for knee pain include arthritis caused by primary osteoarthritis, rheumatoid arthritis, psoriatic arthritis, and secondary arthritis. The surgery is performed when all conservative forms of management are exhausted.
Owing to the success of the surgery, a number of patients are today undergoing total knee replacement. By 2030, knee replacement surgery is projected to grow by 189 percent. Knee pain due to arthritis can be quite debilitating for patients of all age groups. Knee arthroplasty offers excellent pain relief with increased mobility.
Anatomy
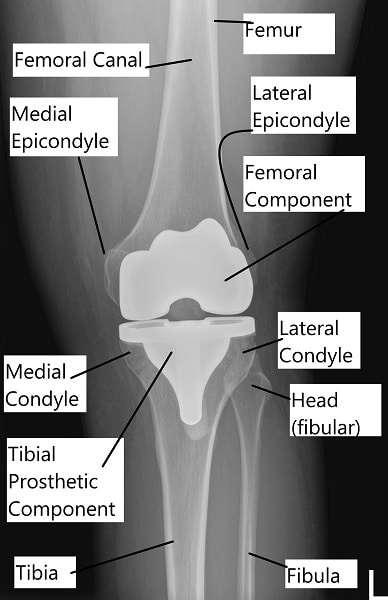
The knee joint is a large synovial hinge joint. The joint is formed by the lower end of the thigh bone (femur) and the upper part of the shinbone (tibia). The kneecap (patella) forms a joint with the lower part of the thigh bone.
Patella acts as a lever for straightening the leg. It also allows smooth gliding of the bones when straightening or bending the leg.
Articulating cartilage is a glistening white smooth tissue covering the end of the bones forming the joint. The cartilage also covers the undersurface of the patella. The cartilage is toughened and flexible to allow smooth gliding of the joint surfaces.
The ligaments surrounding the knee provide stability to the joint. The ligaments providing stability at the front and the back are anterior cruciate ligament and the posterior cruciate ligament. Medial and lateral collateral ligaments provide stability on the sides of the knee joint. Tear or laxity of the ligaments lead to instability and damage the joint.
Meniscus are small pads, one on the inner side and one on the outer side of the knee joint. Both the meniscus cushions the impact on the ends of the bones. They also provide additional stability to the joint. Both the meniscus and the ligaments have limited blood supply.
Synovium is a tissue lining the inner surface of the joint. The synovium secretes a watery thin, clear and sticky fluid known as synovial fluid. Just like machine oil, it acts as a lubricant allowing smooth gliding of the joint. Bursae are small fluid-filled sacs helping in smooth gliding of the structures around the knee joint.
Proper alignment between the femur and tibia is necessary for the distribution of joint forces equally. Muscles crossing the knee joint allow for bending and straightening the knee.
Causes
Arthritis due to variety of reasons remains the most common indication for total knee replacement. Various types of arthritis are primary osteoarthritis, secondary osteoarthritis, rheumatoid arthritis, or psoriatic arthritis.
With growing age, the structures which form the knee joint, including the bones, articular cartilage, tendons, ligaments, meniscus, and muscles degenerate. The changes culminate into tears of the meniscus and cartilage, leading to loss of smooth gliding of the joint. The joint may become inflamed and swollen.
Rheumatoid arthritis is a systemic disease often affecting multiple joints, especially the smaller joints. The knee joint may be affected as well and usually, both the knees may be involved. There is extensive destruction of the cartilage and subchondral bone with inflammation of the synovium. The destruction is carried out by the body’s immune cells recognizing the normal cells as foreign.
Other forms of arthritis such as psoriatic arthritis and gouty arthritis also lead to the destruction of the joint. Arthritis secondary to knee injury is known as secondary osteoarthritis. Injuries such as fractures or tears of the meniscus and ligament may cause incongruity of the joint surface. Young patients with a history of trauma to the injury may present with secondary arthritis.
Congenital or residual deformities while growing such bow legs or knock knees cause malalignment of the joint. The unequal distribution of forces leads to the development of early arthritis.
Symptoms & Management
Patients with advanced arthritis usually present with knee pain. The knee pain is especially aggravated on activities such as walking, squatting, bending, twisting or turning. They experience difficulty navigating stairs and report stiffness after periods of inactivity. Joint crepitus may be experienced which is described as a grinding/popping sensation on moving the knee.
A wide range of conservative management options is tried before knee replacement surgery. These include heat pads, physical therapist visits, weight loss, or glucosamine and chondroitin sulfate tablets. The patient may receive cortisone injections or visco-supplement injections in the knee.
Unfortunately, arthritis is a progressively worsening condition. The conservative management options may thin out and the pain may become more persistent. The patients who have exhausted all conservative treatment options are candidates for knee replacement.
Procedure
Before the procedure, the patients are examined thoroughly for any deformity in the knees. Their medical conditions are assessed for them to be medically fit to undergo the procedure. Routine blood tests and cardiograms are done as a part of presurgical testing. The surgery is usually performed either in general anesthesia or spinal anesthesia.
Cross-matching of the patients’ blood is done for blood transfusion if needed. Any kind of blood thinner is stopped a few days before the procedure. Imaging studies usually an X-ray and sometimes a CT scan may be done to assess the degree of bone loss. Preoperative planning is done to assess the correct biomechanical axis of the knees.
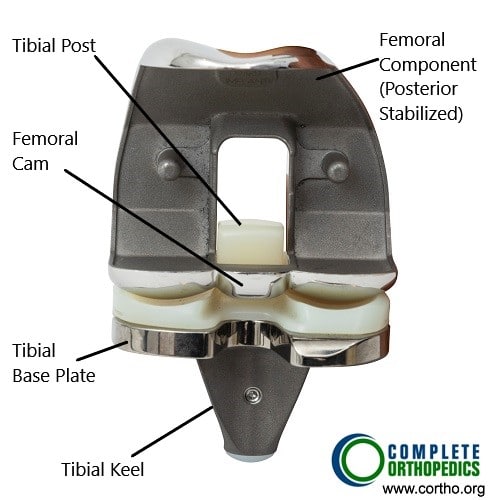
The joint is opened from the front and the damaged bone along with cartilage is removed. Bone cuts are made with specially designed jigs to prepare the joint surface. Both the anterior and posterior cruciate ligaments are usually sacrificed in posterior stabilized implants. The medial and lateral collateral ligaments are retained and surgically released to balance the alignment.
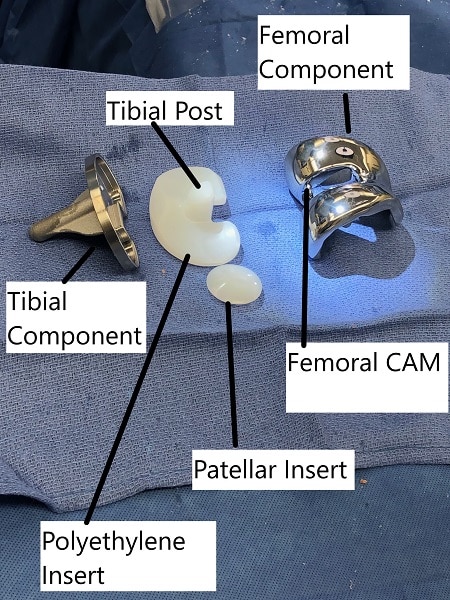
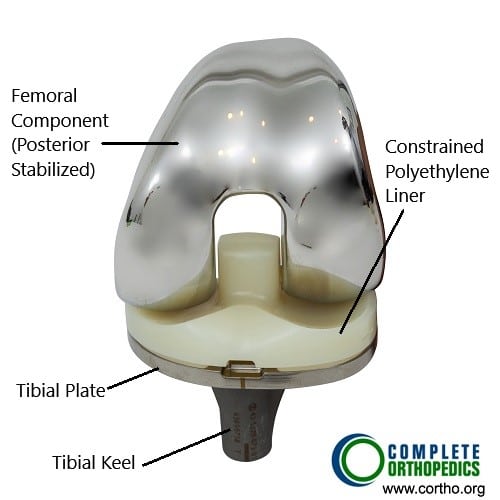
The metal parts are then introduced and are glued with acrylic bone cement. A special high-grade plastic (Polyethylene) is inserted between the metal parts acting as a stabilizer and cushion. The metal parts are made of a cobalt-chromium alloy and are designed to allow smooth gliding. The undersurface of the patella is resurfaced and a special plastic is cemented to the undersurface. The joint is thoroughly irrigated, cleaned and closed. Intraoperative medications may be injected to reduce post-op pain. The patient is shifted to the recovery room where their vitals are closely monitored.
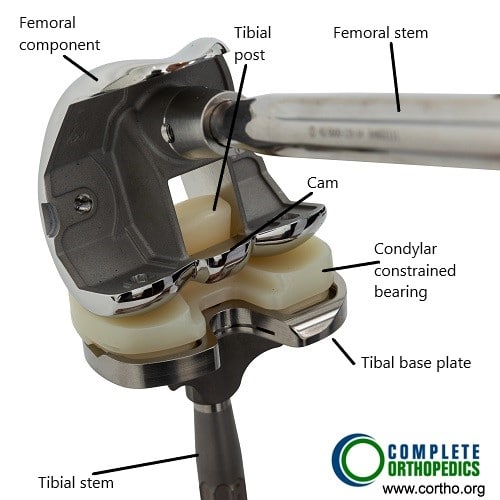
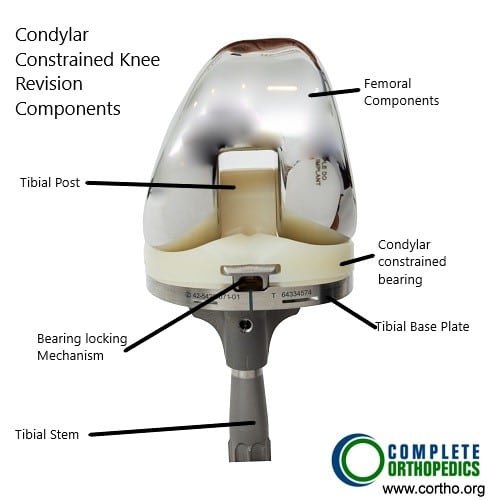
The above images show the prosthetic knee replacement components from the front and the back. The femoral component (posterior stabilized) has a cam mechanism which allows posterior translation of the femur on the tibial post of the bearing surface. The femoral rollback aids in achieving deeper flexion which in a normal knee is done by the knee ligaments. The polyethylene insert is made of highly cross linked polyethylene, which is resistant to wear and tear. The keel of the tibial component is fixed in the upper part of the shin bone using bone cement.
The modular components shown in the images above are used in revision knee surgery or complex knee replacement. Depending upon the knee anatomy and bone loss, the surgeon is able to achieve greater stability of the prosthetic implant using modular components.
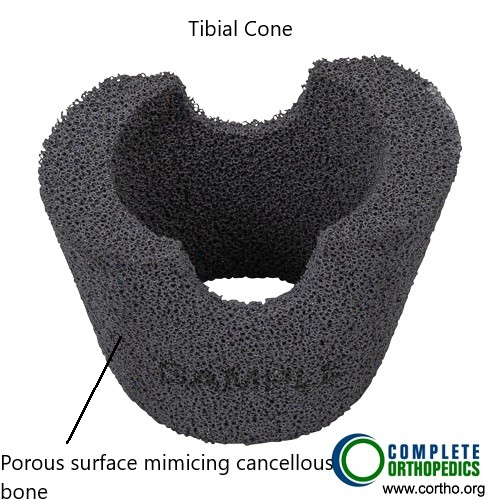
Metal cone resembling trabecular bone may be used to fill in bone gaps encountered in the metaphyseal region intraoperatively. The trabecular surface pattern of the tibial cone ensures biological union of the component.
After the Procedure
The recovery time is expedited and patients are able to walk the same day of the procedure with support. The post-operative pain is managed with medications and usually, a blood thinner is prescribed to prevent blood clots. Physical therapy is initiated to regain strength and increase flexibility.
Most patients are able to go home the day after surgery. The patients are able to walk without support usually in 8-12 weeks. They are able to resume their daily activities. X-rays are taken of the artificial knee/replaced knee to check for proper alignment and fixation.
They are able to walk, climb stairs, bend, ride a bicycle, drive a car and climb stairs without any limitation. The patients are advised not to undergo any high impact activities such as running or jumping.
Possible complications
As true with any major surgery, they may be potential complications with a joint replacement surgery. There may be medical complications such as heart attack, stroke, or pneumonia. There may be intraoperative complications such as fractures, shortening, instability, nerve or blood vessel damage.
During the few weeks after the surgery, there is an increased risk of blood clots in the leg, infection or dislocation. In the following months, the patient may complain of persistent pain, a clunk while moving the knee, dislocation or stiffness. In the long run, there may be loosening of the implant or the plastic component may wear off.
Success
On average, a total knee replacement lasts for more than 15- 20 years, for some patients, it may last their lifetime. Owing to the success, total knee replacement surgeries are being performed regularly. The patients express satisfaction in being able to get back to their daily activities. They are pain-free and report greater range of motion.
Do you have more questions?
How soon after knee replacement surgery can complications typically arise?
Complications after knee replacement surgery can arise at various times during the postoperative period, ranging from the immediate postoperative period to months or even years after surgery. It’s essential to remain vigilant for signs and symptoms of complications and seek prompt medical attention if any concerns arise.
Are there any specific precautions or considerations for patients with certain medical conditions (e.g., diabetes, heart disease) undergoing knee replacement surgery?
Patients with medical conditions may require additional preoperative evaluation and optimization to reduce the risk of complications during and after knee replacement surgery. Close coordination between the orthopedic surgeon and other medical specialists is essential to ensure safe and successful outcomes.
What factors should patients consider when selecting a surgeon and hospital for knee replacement surgery?
Patients should consider factors such as surgeon experience, hospital reputation, surgical volume, complication rates, patient satisfaction scores, and access to comprehensive pre- and post-operative care when choosing where to undergo knee replacement surgery.
How does prehabilitation (pre-operative rehabilitation) contribute to better outcomes following knee replacement surgery, and what exercises are typically included in prehabilitation programs?
Prehabilitation aims to optimize patients’ physical and mental health before surgery, leading to improved post-operative recovery and functional outcomes. Exercises often include strengthening, flexibility, and cardiovascular conditioning tailored to individual needs.
What are the potential risks and benefits of simultaneous bilateral knee replacement surgery compared to staged procedures?
Simultaneous bilateral knee replacement offers the advantage of a single anesthesia exposure and shorter overall recovery time but may carry increased risks such as higher blood loss and complications related to immobility.
Are there any emerging technologies or advancements in knee replacement surgery that patients should be aware of?
Emerging technologies such as patient-specific implants, 3D printing, and advanced surgical navigation systems are being explored to further improve the precision and outcomes of knee replacement surgery.
What are the potential risks and complications associated with knee replacement surgery?
Knee replacement surgery, like any surgical procedure, carries risks such as infection, blood clots, nerve damage, implant failure, stiffness, and persistent pain.
How long does it typically take to recover from knee replacement surgery, and what is the rehabilitation process like?
Recovery time can vary, but most patients undergo several weeks of physical therapy to regain strength, mobility, and function in the replaced knee.
Are there any restrictions or limitations on activities following knee replacement surgery?
While patients can typically resume low-impact activities like walking and swimming, high-impact activities such as running and jumping may be discouraged to prevent implant wear and tear.
What factors determine the success rate of knee replacement surgery, and how can patients optimize their outcomes?
Success rates depend on factors such as patient age, overall health, severity of knee damage, surgical technique, implant selection, and adherence to post-operative rehabilitation protocols.
Are there alternatives to traditional knee replacement surgery, such as partial knee replacement or minimally invasive procedures?
Yes, alternatives include partial knee replacement for localized knee arthritis and minimally invasive techniques that aim to preserve more healthy tissue and facilitate quicker recovery.
What is the role of robotic-assisted surgery in knee replacement procedures, and how does it differ from traditional approaches?
Robotic-assisted surgery utilizes advanced technology to enhance precision and accuracy in implant placement, potentially improving outcomes and reducing complications compared to traditional techniques.
Can knee replacement surgery be performed on both knees simultaneously, or is it typically done one at a time?
While simultaneous bilateral knee replacement can be considered for select patients, most individuals undergo staged procedures, addressing one knee at a time to minimize post-operative complications and facilitate rehabilitation.
How long do knee implants typically last, and what factors can affect their longevity?
Knee implants can last 15-20 years or longer, but their durability may be influenced by factors such as patient activity level, implant design, material quality, and surgical technique.
Can knee replacement surgery be performed in younger patients, and are there any special considerations for this population?
Knee replacement in younger patients may present challenges due to the need for long-term implant durability and potential revision surgeries over their lifetime. Careful patient selection and counseling are essential.
What are the potential complications of delaying knee replacement surgery, and when is the optimal time to consider surgery?
Delaying surgery may lead to worsening pain, functional limitations, joint deformity, and compromised outcomes. The optimal timing for surgery depends on the individual’s symptoms, functional status, and response to conservative treatments.
Are there any lifestyle modifications or preventive measures that can help delay or minimize the need for knee replacement surgery?
Lifestyle modifications such as weight management, regular exercise, joint protection techniques, and appropriate footwear may help alleviate knee pain and delay the progression of arthritis, reducing the need for surgery.
What are the differences between total knee replacement and partial knee replacement, and how is the appropriate procedure determined?
Total knee replacement involves replacing the entire knee joint, while partial knee replacement addresses only the damaged compartment. The choice between procedures depends on the extent and location of arthritis and the patient’s anatomy.
What types of anesthesia are used for knee replacement surgery, and what are the associated risks and benefits?
Knee replacement surgery can be performed under general anesthesia, regional anesthesia (such as spinal or epidural), or a combination of both. The choice depends on patient factors and surgical preferences, with each option carrying its own risks and benefits.
Are there any factors that may increase the risk of complications or adverse outcomes following knee replacement surgery?
Factors such as advanced age, obesity, smoking, diabetes, heart disease, and certain medications may increase the risk of complications and warrant careful preoperative evaluation and optimization.
What are the most common reasons for knee replacement revision surgery, and how are complications addressed?
Reasons for revision surgery include infection, implant loosening, instability, wear and tear, and persistent pain. Revision procedures aim to address complications and restore function, often requiring more complex surgical techniques.
How does the choice of implant type (e.g., fixed-bearing vs. mobile-bearing) affect outcomes and longevity in knee replacement surgery?
Implant selection depends on factors such as patient age, activity level, and surgeon preference. Both fixed-bearing and mobile-bearing designs have shown favorable outcomes, with differences in wear patterns and range of motion.
Are there any complementary or alternative therapies that can help manage knee pain and improve function without surgery?
Complementary therapies such as acupuncture, massage, physical therapy, and dietary supplements may provide symptomatic relief and improve joint function, although their efficacy varies among individuals.
How does knee osteoarthritis differ from other types of arthritis, and what are the treatment options specific to this condition?
Knee osteoarthritis is characterized by the breakdown of cartilage in the knee joint, leading to pain, stiffness, and loss of function. Treatment options include lifestyle modifications, medications, injections, physical therapy, and surgical interventions like knee replacement.
Can knee injuries such as ACL tears or meniscus tears be effectively treated without surgery, and what factors influence the decision for surgical intervention?
While some knee injuries may heal with conservative measures like rest, physical therapy, and bracing, surgical intervention may be necessary for severe or unstable injuries that compromise joint stability and function. Individualized treatment plans are based on factors such as the severity of injury, patient activity level, and treatment goals.
My name is Dr. Suhirad Khokhar, and am an orthopaedic surgeon. I completed my MBBS (Bachelor of Medicine & Bachelor of Surgery) at Govt. Medical College, Patiala, India.
I specialize in musculoskeletal disorders and their management, and have personally approved of and written this content.
My profile page has all of my educational information, work experience, and all the pages on this site that I've contributed to.